Psychological Interventions for Chronic Health Disorders
Most chronically ill patients achieve a fairly high quality of life. However, adverse effects of chronic disease and treatments have led health psychologists to develop psychological interventions to ameliorate these problems. Because anxiety and depression are intermittently high among chronically ill patients, an evaluation for these problems needs to be a standard part of chronic care. Patients who have a history of depression or other mental illness prior to the onset of their chronic illness are at particular risk and so should be evaluated early for potential interventions.

Chronic Diseases
Read More- Counseling for Cancer
Pharmacological – Psychological Interventions
Pharmacological treatment may be appropriate for patients suffering from depression associated with chronic illness. They commonly prescribe antidepressants under such circumstances. Treatment with any substance, other than food, to prevent, diagnose, treat, or relieve symptoms of a disease or abnormal condition.
1. Individual Therapy
Individual therapy is one of the common psychological interventions for patients who have psychosocial complications due to chronic illness. But there are important differences between psychotherapy with medical patients and psychotherapy with patients who have primarily psychological disorders.
- First, therapy with medical patients is more likely to be episodic than continuous. Chronic illness raises crises and issues intermittently that may require help. For example, recurrence or worsening of a condition may present a crisis that needs to be addressed with a therapist.
- Second, collaboration with the patient’s physician and family members is critical. The physician can inform the psychologist or other counselor of a patient’s current physical condition.
- Third, therapy with medical patients requires respect for patients’ defenses. In traditional psychotherapy, one of the therapist’s goals may be to challenge a patient’s defenses that may interfere with an adequate understanding of his or her problems. However, in the case of chronically ill patients, these defenses may serve a benign function in protecting them from the full realization of the ramifications of their disease.
- Fourth, the therapist working with a medical patient must have a comprehensive understanding of the patient’s illness and its modes of treatment. Illness and treatments themselves produce psychological problems (for example, depression due to chemotherapy), and a therapist who is ignorant of this fact may make incorrect interpretations.
Coping skills training can improve functioning for chronic diseases. Such programs can increase knowledge about the disease, reduce anxiety, increase patients’ feelings of purpose and meaning in life.
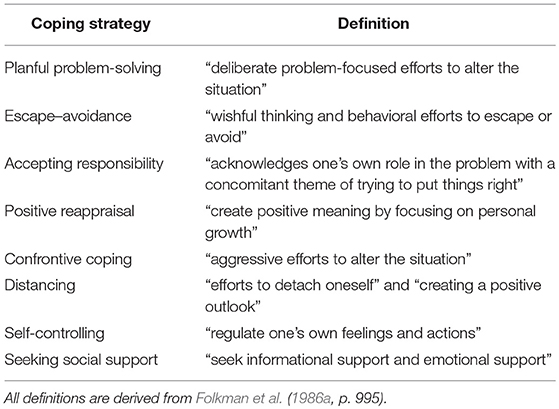
Coping Strategies
2. Relaxation, Stress Management, and Exercise
Relaxation training is a widely used intervention with the chronically ill, including asthmatics, cancer patients, and multiple sclerosis patients, among others. Combining relaxation training with stress management and blood pressure monitoring has proven useful in the treatment of hypertension. Mindfulness-based stress reduction (MBSR) can improve adjustment to chronic illness. Mindfulness meditation teaches people to be highly aware and focused on the present moment, accepting and acknowledging thoughts and feelings without becoming distracted or distressed by stress.

Progressive Muscle Relaxation
3. Social Support Interventions
Social support is an important resource for people with chronic illnesses. The benefits of social support have been found for virtually every chronic illness in which this resource has been examined including cancer, spinal cord injury, end-stage renal disease, and cardio- vascular disease.
4. Family Support
Family support is especially important. It enhances the patient’s physical and emotional functioning, it promotes adherence to treatment and it can improve course of illness.
Family members can remind the patient about activities that need to be undertaken and even participate in them, so that adherence is more likely. For example, the family may take a daily jog through the neighborhood just before breakfast or dinner.
Sometimes family members need guidance in the well-intentioned actions they should avoid because such actions actually make things worse. For example, some family members think they should encourage a chronically ill patient to be relentlessly cheerful, which can have the unintended effect of leaving the patient unable to share distress or concerns with others.
5. Support Groups
Social support groups represent a resource for the chronically ill. A therapist initiated some of these groups, and in some cases, they are patient led. Support groups also discusses issues of mutual concern that arise as a consequence of illness.
However, they provide specific information about how others have dealt with the problems. And give people an opportunity to share their emotional responses with others facing the same problems.
Social support groups can satisfy unmet needs for social support from family and care givers. Moreover, they may act as an additional source of support provided by those going through the same event. Despite advances in care for the chronically ill, medical and psychosocial care for the chronically ill is still irregular. As the burden on caregivers clearly attests.
References
Taylor, Shelley E. (2018). Health Psychology (10th Ed). McGraw Hill Higher Education. Indian Edition
Subscribe to Careershodh
Get the latest updates and insights.
Join 18,509 other subscribers!
Niwlikar, B. A. (2022, March 25). 5 Psychological Interventions for Chronic Health Disorders. Careershodh. https://www.careershodh.com/psychological-interventions-for-chronic-health-disorders/
