Introduction
Patient-Provider relationship is one of the most crucial aspects of medical practice. It determines treatment adherence, patient satisfaction, and overall health outcomes (Taylor, 2013). Effective communication is central to this relationship, ensuring accurate diagnosis, shared decision-making, and positive healthcare experiences. However, communication barriers such as jargon, time constraints, stereotyping, and patient anxiety often lead to misunderstandings, dissatisfaction, and non-adherence to treatment.
Read More- Health Psychology
The Shift from Passive to Active Patients
Historically, healthcare systems followed a paternalistic model, where physicians held complete authority over medical decisions, and patients passively accepted their recommendations. However, modern healthcare has shifted toward a patient-centered approach, emphasizing collaborative decision-making (Taylor, 2013).
Factors influencing this shift include:
- Increased access to health information through the internet and social media.
- Rise in chronic diseases, requiring long-term patient involvement in care.
- Advancements in medical technology, offering multiple treatment choices.
- Legal and ethical emphasis on patient autonomy in medical decision-making.
A patient-centered approach improves health outcomes by fostering trust, satisfaction, and engagement in treatment plans.
Adherence to Treatment
Consumerism in Healthcare
Patients today view healthcare as a service industry and demand quality, efficiency, and transparency. This “healthcare consumerism” has led to:
- Increased expectations for personalized care.
- A demand for shared decision-making.
- A focus on holistic health, including mental and emotional well-being.
The shift from doctor-centered to patient-centered care underscores the importance of effective communication in fostering trust and adherence.
Types of Healthcare Models
The healthcare delivery system affects the quality of patient-provider communication.
1. Health Maintenance Organizations (HMOs)
- Patients must select a primary care provider (PCP) from a limited network.
- Specialist visits require preauthorization, leading to delays in care.
- Cost-effective but may reduce personalization of care (Taylor, 2013).
2. Preferred Provider Organizations (PPOs)
- Greater patient autonomy in choosing providers.
- No referrals required for specialists.
- More expensive but offers better continuity of care.
3. Patient Dissatisfaction in Managed Care
The shift towards managed care models has reduced consultation times and increased bureaucracy, negatively impacting patient-provider communication. Short visits (12–15 minutes) and financial incentives for referrals contribute to a lack of continuity in patient care (Taylor, 2013).

Adherence to Treatment
Provider-Related Barriers to Communication
Some barriers to communication from the provider’s side include-
- Inattentiveness- Physicians often interrupt patients within the first 23 seconds (Simon, 2003). Lack of active listening results in incomplete medical histories and misdiagnosis.
- Medical Jargon- Providers often use complex medical terms, leading to confusion and misunderstanding. Patients may hesitate to ask for clarification due to fear of seeming uninformed.
- Depersonalization- Some doctors treat patients as cases rather than individuals, reducing trust and engagement (Zimbardo, 1969).
- Stereotyping Patients- Racial and socioeconomic biases result in disparities in medical care (van Ryn & Fu, 2003). Elderly patients often receive less aggressive treatments compared to younger patients (Haug & Ory, 1987).
Patient-Related Barriers to Communication
Some barriers to communication from the patient’s side include-
- Anxiety and Stress- High anxiety impairs cognitive processing, reducing information retention (Graugaard & Finset, 2000).
- Health Illiteracy- Many patients lack the skills to understand medical advice, leading to poor adherence (Galesic et al., 2009).
- Mismatched Expectations- Patients may expect medications for all symptoms, while doctors may prioritize lifestyle changes.
Consequences of Poor Communication
The consequences of poor communication include-
- Non-Adherence to Treatment- Statistics on Non-Adherence
- 33% of patients fail to complete antibiotics.
- 50–60% ignore behavioral change advice (e.g., quitting smoking).
- 85% of patients do not take medication as prescribed (O’Connor, 2006).
2. Creative Non-Adherence– Some patients alter dosages or mix treatments based on personal beliefs (Wroe, 2001).
3. Malpractice Cases– Many lawsuits arise not from medical errors but from poor communication (Reitman, 2003).
Strategies for Improving Patient-Provider Communication
Some strategies to improve patient provider communication include-
1. Training Healthcare Providers
- Use simple language and avoid jargon.
- Encourage patients to ask questions.
- Confirm patient understanding by having them repeat instructions.
- Use nonverbal cues to convey empathy (Guéguen et al., 2010).
2. Training Patients
- Prepare questions before appointments.
- Take notes during visits.
- Bring a companion for support.
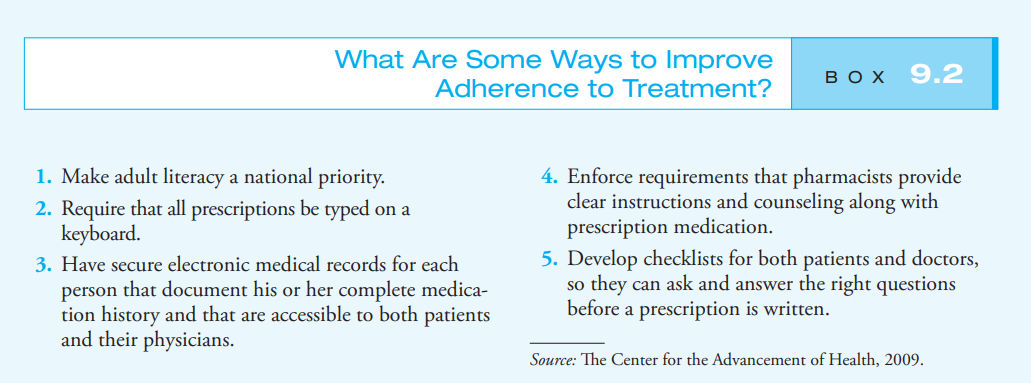
3. Addressing Barriers to Adherence
- Set realistic health goals and provide motivation.
- Use reminders like mobile alerts.
- Encourage shared decision-making.
Information-Motivation-Behavioral Skills (IMB) Model
Health behavior adherence depends on three factors (Fisher & Fisher, 1992)-

Information-Motivation-Behavioral Skills Model of Health Behavior
- Information – Patients need clear, accurate knowledge.
- Motivation – Emotional and psychological engagement in care.
- Behavioral Skills – The ability to implement medical advice.
Conclusion
The patient-provider relationship is the foundation of effective healthcare. Clear communication, trust, and shared decision-making enhance patient satisfaction and adherence to treatment. Both providers and patients play a role in improving communication, and training programs for physicians and public health initiatives can significantly improve healthcare interactions.
References
Taylor, S. E. (2013). Health Psychology. McGraw-Hill.
Fisher, W. A., & Fisher, J. D. (1992). The Information-Motivation-Behavioral Skills Model of Health Behavior Change.
Simon, H. (2003). Patient-Physician Interaction Times.
van Ryn, M., & Fu, S. S. (2003). Racial and Ethnic Disparities in Health Care.
Wroe, A. L. (2001). Adherence to Treatment: Psychological Influences.
Subscribe to Careershodh
Get the latest updates and insights.
Join 18,513 other subscribers!
Niwlikar, B. A. (2025, February 28). Patient-Provider Relationship and 3 Important Strategies to Improve Communication. Careershodh. https://www.careershodh.com/patient-provider-relationship/
