Introduction
Neurocognitive disorders (NCDs) and delirium represent a group of conditions characterized by acquired cognitive decline that interferes with independence in everyday functioning. Unlike neurodevelopmental disorders, neurocognitive disorders involve deterioration from a previously achieved level of cognitive functioning. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies these conditions under Delirium and Major and Mild Neurocognitive Disorders (American Psychiatric Association, 2013).
These disorders affect multiple cognitive domains including memory, attention, language, executive functioning, perceptual-motor abilities, and social cognition. Neurocognitive disorders may be acute and reversible, as in delirium, or chronic and progressive, as in dementia-related conditions such as Alzheimer’s disease. With increasing life expectancy worldwide, neurocognitive disorders have become a major public health concern, affecting not only patients but also caregivers, healthcare systems, and society at large.
Read More: Substance Abuse Disorder
Delirium
Delirium is an acute, fluctuating disturbance in attention, awareness, and cognition, usually caused by an underlying medical condition, substance intoxication or withdrawal, infection, or metabolic imbalance. It develops over a short period (hours to days) and represents a medical emergency requiring immediate intervention (APA, 2013).
Delirium
Diagnostic Criteria (DSM-5)
Delirium is diagnosed based on the following criteria:
- Disturbance in attention and awareness: Reduced ability to focus, sustain, or shift attention and decreased orientation to the environment.
- Acute onset and fluctuating course: Symptoms develop rapidly and fluctuate throughout the day.
- Additional cognitive disturbance: Memory deficits, disorientation, language impairment, or perceptual disturbances.
- Not better explained by another neurocognitive disorder: Symptoms are not solely attributable to dementia or coma.
- Evidence of a physiological cause: Medical condition, substance intoxication or withdrawal, or exposure to toxins.
Types of Delirium
- Hyperactive Delirium – agitation, restlessness, hallucinations.
- Hypoactive Delirium – lethargy, reduced alertness, withdrawal.
- Mixed Delirium – alternating hyperactive and hypoactive states.
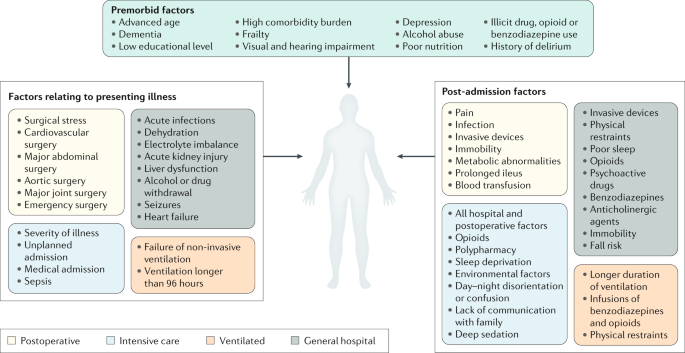
Causes and Risk Factors
- Infections (e.g., urinary tract infections, pneumonia)
- Electrolyte imbalance
- Medication toxicity
- Alcohol or drug withdrawal
- Post-surgical complications
- Advanced age and pre-existing cognitive impairment
Treatment of Delirium
- Identification and treatment of the underlying cause
- Environmental stabilization (quiet room, reorientation cues)
- Hydration and nutritional support
- Low-dose antipsychotics (only if severe agitation or psychosis is present)
Delirium is often reversible if treated promptly.
Major Neurocognitive Disorders (Dementia)
Major Neurocognitive Disorder (formerly dementia) involves significant cognitive decline in one or more cognitive domains that interferes with independence in daily activities. The decline is gradual, progressive, and usually irreversible.
1. Alzheimer’s Disease (AD)
Alzheimer’s disease is the most common cause of major neurocognitive disorder, accounting for approximately 60–70% of cases. It is a progressive, degenerative brain disorder primarily affecting memory and learning before spreading to other cognitive functions.
Diagnostic Features
- Gradual onset and progressive decline
- Prominent memory impairment, especially recent memory
- Language difficulties (aphasia)
- Impaired executive functioning
- Disorientation to time and place
- Personality and behavioral changes
Neuropathology
- Beta-amyloid plaques disrupting neuronal communication
- Neurofibrillary tangles (tau protein) causing neuronal death
- Widespread cortical atrophy

Alzheimer’s Disease
Causes and Risk Factors
- Advanced age
- Genetic predisposition (APOE-ε4 allele)
- Family history
- Cardiovascular risk factors
- Low cognitive reserve
Treatment
- Cholinesterase inhibitors (donepezil, rivastigmine)
- NMDA receptor antagonists (memantine)
- Cognitive stimulation therapy
- Caregiver education and support
No cure exists, but treatment slows symptom progression.
2. Lewy Body Disease (LBD)
Lewy Body Disease is characterized by abnormal protein deposits (Lewy bodies) in the brain. It shares features of both Alzheimer’s disease and Parkinson’s disease.
Diagnostic Features
- Fluctuating cognition and alertness
- Recurrent visual hallucinations
- Parkinsonian motor symptoms (rigidity, tremors)
- REM sleep behavior disorder
- Sensitivity to antipsychotic medications
Causes
- Accumulation of alpha-synuclein protein
- Neurodegeneration affecting cortical and subcortical regions
Treatment
- Cholinesterase inhibitors for cognition
- Dopaminergic medications (with caution)
- Avoidance of typical antipsychotics
3. Vascular Neurocognitive Disorder
Vascular Neurocognitive Disorder results from cerebrovascular disease, including strokes and chronic ischemia, leading to impaired blood flow to the brain.
Diagnostic Features
- Stepwise cognitive decline
- Impaired attention and executive functioning
- Emotional lability
- Motor weakness
Causes
- Stroke
- Hypertension
- Diabetes
- Atherosclerosis
Treatment
- Management of vascular risk factors
- Antiplatelet therapy
- Cognitive rehabilitation
- Lifestyle modifications
4. Neurocognitive Disorder due to Traumatic Brain Injury (TBI)
This disorder occurs following head trauma resulting in cognitive, emotional, and behavioral impairments.
Diagnostic Features
- Memory and attention deficits
- Executive dysfunction
- Personality changes
- Emotional dysregulation
Causes
- Road traffic accidents
- Sports injuries
- Falls
- Assaults
Treatment
- Neurorehabilitation
- Cognitive therapy
- Behavioral management
- Occupational therapy
5. Parkinson’s Disease Neurocognitive Disorder
Parkinson’s disease is a neurodegenerative movement disorder that may progress to major neurocognitive disorder.
Diagnostic Features
- Bradykinesia, rigidity, tremors
- Cognitive slowing
- Impaired executive functioning
- Depression and anxiety
Causes
- Dopamine depletion in the substantia nigra
- Alpha-synuclein accumulation

Parkinson’s Disease
Treatment
- Dopaminergic medications
- Cognitive rehabilitation
- Psychotherapy for mood symptoms
6. Huntington’s Disease
Huntington’s disease is a genetic, autosomal dominant disorder characterized by progressive motor, cognitive, and psychiatric deterioration.
Diagnostic Features
- Chorea (involuntary movements)
- Cognitive decline
- Personality changes
- Depression and psychosis
Causes
- Mutation in the HTT gene
- Progressive neuronal loss in basal ganglia
Treatment
- Symptomatic management
- Antipsychotics for chorea
- Antidepressants
- Genetic counseling
Conclusion
Delirium and major neurocognitive disorders represent a diverse group of conditions affecting cognition, behavior, and functioning. While delirium is often reversible with prompt treatment, most major neurocognitive disorders are progressive and require long-term management. Early diagnosis, accurate differentiation among subtypes, and comprehensive care strategies significantly improve quality of life for patients and caregivers. As populations age globally, addressing neurocognitive disorders remains a critical priority in mental health and medical practice.
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Puri, B. K., Laking, P. J., & Treasaden, I. H. (1996). Textbook of Psychiatry. Churchill Livingstone.
Butcher, J. N., Hooley, J. M., & Mineka, S. (2014). Abnormal Psychology (15th ed.). Pearson.
Carson, R. C., Butcher, J. N., & Mineka, S. (2007). Abnormal Psychology (13th ed.). Pearson.
Nevid, J. S., Rathus, S. A., & Greene, B. (2014). Abnormal Psychology (9th ed.). Pearson.
World Health Organization. (2019). ICD-11: International Classification of Diseases.
Niwlikar, B. A. (2025, December 15). 6 Important Delirium and Neurocognitive Disorders. Careershodh. https://www.careershodh.com/delirium-and-neurocognitive-disorders/
