Introduction
Cluster-B personality disorders constitute one of the most widely studied and clinically challenging groups within the DSM-5 classification. They are commonly described as the dramatic, emotional, and erratic cluster, reflecting the intense emotional reactivity, impulsive behavior, unstable relationships, and disruptive interpersonal patterns typically observed in affected individuals. Cluster-B disorders include:
- Antisocial Personality Disorder (ASPD)
- Borderline Personality Disorder (BPD)
- Histrionic Personality Disorder (HPD)
- Narcissistic Personality Disorder (NPD)
These disorders often create significant distress for both individuals and those around them, especially due to emotional dysregulation, perceived manipulation, interpersonal instability, and extreme impulsivity. Cluster-B disorders frequently co-occur with mood disorders, trauma histories, substance abuse, suicidal behavior, and self-harm. They typically emerge in adolescence or early adulthood and may persist across the lifespan, although some symptoms such as impulsivity tend to decline with age.
Read More: Psychodynamics
General Characteristics of Cluster-B Disorders
Although each disorder presents with unique and specific symptoms, several overarching features unify this cluster.
- Emotional Intensity and Dysregulation: Individuals often experience emotions with extreme intensity. Their affect may shift abruptly, feel overwhelming, or result in impulsive behavior. They often struggle to regulate anger, shame, fear of abandonment, or euphoria.
- Impulsivity and Risk-taking Behavior: Many individuals engage in impulsive actions such as reckless driving, substance use, unprotected sex, binge eating, gambling, or sudden aggressive confrontation.
- Unstable or Chaotic Relationships: A hallmark of Cluster-B disorders is the inability to maintain stable relationships due to mistrust, dependency, jealousy, manipulation, or idealization–devaluation cycles.
- Distortions in Self-Image: Whether it is inflated self-importance (NPD), unstable self-concept (BPD), or excessive need for approval (HPD), distorted self-perception is central.
- Behavioral Dramaticness and Attention-Seeking: Some individuals exhibit dramatic and expressive behaviors to gain attention, maintain control, or fulfill emotional needs.
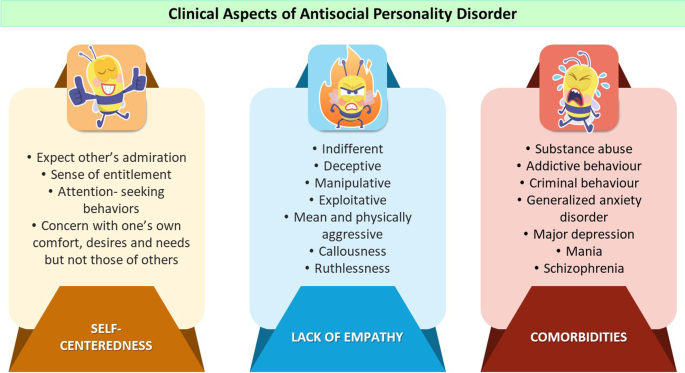
1. Antisocial Personality Disorder (ASPD)
ASPD involves a pervasive pattern of disregard for, and violation of, the rights of others beginning in childhood or early adolescence and continuing into adulthood. The DSM-5 specifies that individuals must be at least 18 years old and have a history of conduct disorder before age 15.
Anti-Social Personality Disorder
Diagnostic Features
Some diagnostic features include:
- Failure to Conform to Social Norms: Repeated engagement in unlawful behavior, disregard for rules, and violation of societal standards.
- Deceitfulness: Habitual lying, use of aliases, manipulation for personal profit or pleasure.
- Impulsivity: Inability to plan ahead or consider consequences; decisions are made quickly and recklessly.
- Irritability and Aggressiveness: Frequent fights, aggression, and short temper.
- Reckless Disregard for Safety: Engaging in dangerous behaviors without concern for self or others.
- Consistent Irresponsibility: Failure to maintain work behavior or financial obligations.
- Lack of Remorse: Indifference to hurting others or rationalization of harmful acts.
Causes and Risk Factors
Some causes include:
- Genetic Influences: Twin studies suggest strong heritability, especially for callous-unemotional traits.
- Neurobiological Factors: Under-arousal of the autonomic nervous system, reduced fear response, and abnormalities in prefrontal cortex responsible for impulse control.
- Childhood Environment: Severe neglect, physical or emotional abuse, inconsistent discipline, parental antisocial behavior, and exposure to violence
- Conduct Disorder: ASPD almost always emerges from early conduct problems.
Treatment
ASPD is among the most treatment-resistant disorders.
- Cognitive-Behavioral Therapy: Focuses on modifying antisocial behaviors, promoting empathy, and increasing self-control.
- Multisystemic Therapy (MST): Effective in youth with conduct problems, involving family, school, and community.
- Anger Management Programs: Helps manage aggression and impulsivity.
- Substance Abuse Treatment: Important due to high comorbidity. No medication specifically treats ASPD, but mood stabilizers (e.g., lithium) may reduce aggression.
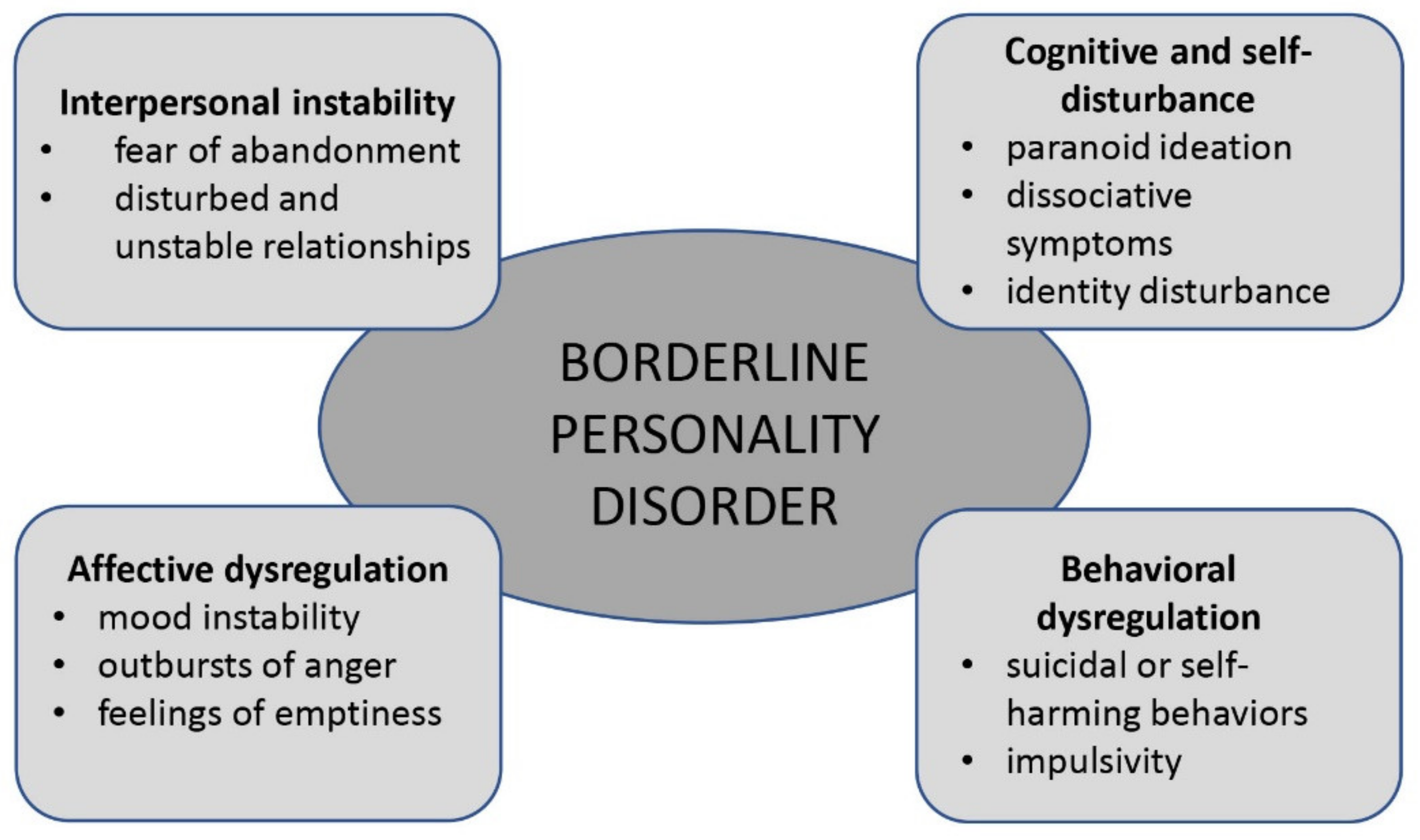
2. Borderline Personality Disorder (BPD)
BPD is characterized by pervasive instability in relationships, self-image, emotion regulation, and impulse control. It is among the most clinically significant personality disorders due to high rates of self-harm and suicide attempts.
Borderline Personality Disorder
Diagnostic Features
Some diagnostic features include:
- Fear of Abandonment: Intense efforts to avoid real or imagined rejection.
- Unstable and Intense Relationships: Alternating between idealization (“you’re perfect”) and devaluation (“you never cared”).
- Identity Disturbance: Unstable self-image, shifting goals, or confusion about values.
- Impulsivity: Risky behaviors such as self-harm, unsafe sex, spending sprees, or substance abuse.
- Recurrent Suicidality or Self-Mutilation: Cutting, burning, and suicide attempts.
- Affective Instability: Extreme mood shifts lasting hours or days.
- Chronic Feelings of Emptiness: A consistent sense of inner void.
- Inappropriate, Intense Anger: Difficulty controlling rage.
- Transient Paranoia or Dissociation: Stress-induced paranoia or depersonalization.
Causes and Risk Factors
Some causes and risk factors include:
- Genetic Factors: Studies indicate strong heritability of emotional instability.
- Trauma and Attachment Issues: BPD is strongly linked to childhood: emotional neglect, physical or sexual abuse, inconsistent caregivers, and invalidating environments (Linehan)
- Emotional Sensitivity: Temperamental vulnerability leading to exaggerated emotional reactions.
- Neurobiological Factors: limbic system hyperreactivity, serotonin dysfunction, and reduced prefrontal regulation
- Biosocial Theory (Linehan): BPD arises from the interaction between biological emotional vulnerability and an invalidating social environment.
Treatment
Unlike ASPD, BPD is highly treatable.
- Dialectical Behavior Therapy (DBT): The gold-standard treatment; focuses on: emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness.
- Mentalization-Based Therapy (MBT): Develops capacity to reflect on one’s own and others’ mental states.
- Transference-Focused Psychotherapy (TFP): Targets identity integration in the therapeutic relationship.
- Schema Therapy: Addresses deep maladaptive schemas such as abandonment and mistrust.
- Medications: No drug cures BPD but may treat symptoms: mood stabilizers: aggression, impulsivity, SSRIs: mood swings, and atypical antipsychotics: paranoia, dissociation
3. Histrionic Personality Disorder (HPD)
HPD involves excessive emotionality and attention-seeking behavior. Individuals with HPD desire to be the center of attention, often through physical appearance, dramatic expression, or exaggerated emotions.

Histrionic Personality Disorder
Diagnostic Features
Some diagnostic features include:
- Discomfort When Not the Center of Attention: They feel unimportant or anxious when ignored.
- Inappropriate Seductiveness: Flirtatious or provocative behavior even in professional settings.
- Rapidly Shifting Emotions: Exaggerated but shallow emotional expression.
- Use of Appearance for Attention: Dramatic clothes, makeup, and gestures.
- Dramatic and Theatrical Speech: Emotional, impressionistic, lacking detail.
- Easily Influenced by Others: High suggestibility and dependence on approval.
- Overestimation of Relationships: Believing relationships are more intimate than they are.
Causes and Risk Factors
Some causes include:
- Temperamental Influences: High sociability and emotional expressiveness.
- Inconsistent Parenting: Overindulgence combined with conditional affection.
- Reinforcement of Dramatic Behavior: Children rewarded for theatrics may internalize this as a strategy to gain attention.
- Cultural Influences: Some cultures may reinforce emotional expressiveness differently.
Treatment
Some treatments include:
- Psychodynamic Therapy: Explores underlying motives for attention-seeking and relationship patterns.
- Cognitive-Behavioral Therapy: Targets distorted thinking, reduces need for approval, and develops problem-solving skills.
- Interpersonal Therapy: Improves social boundaries and communication skills. Medication is not commonly required unless treating depression or anxiety.
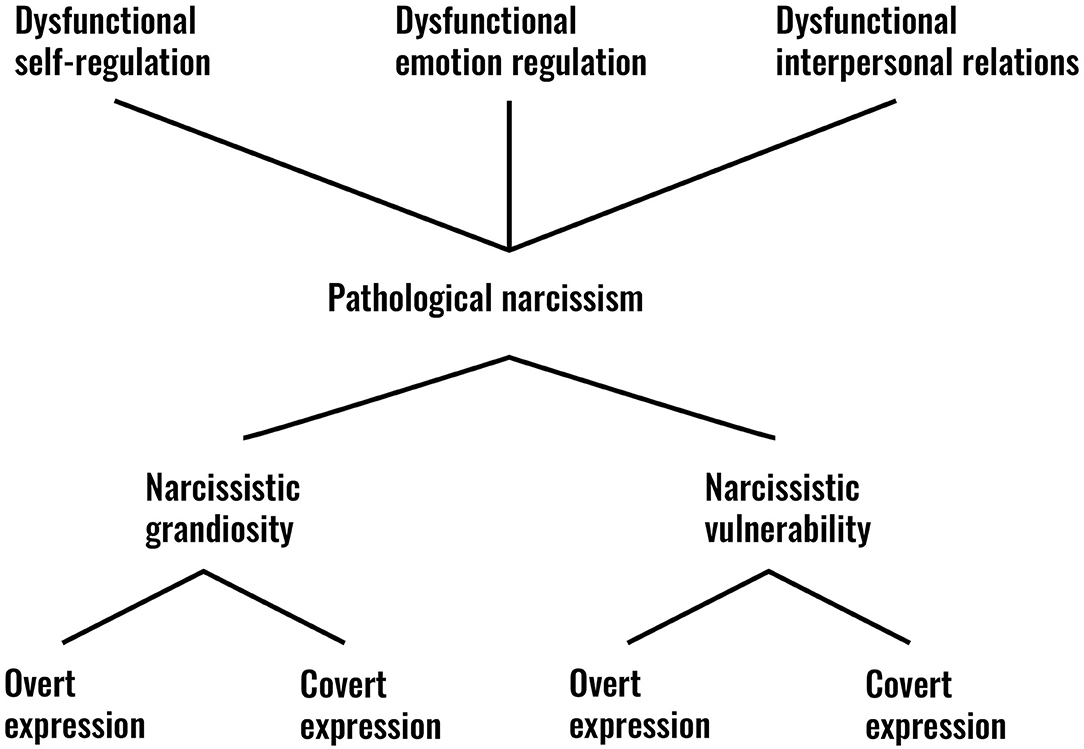
4. Narcissistic Personality Disorder (NPD)
NPD involves a pervasive pattern of grandiosity, need for admiration, and lack of empathy. Despite outward confidence, individuals may have fragile self-esteem.
Narcissistic Personality Disorder
Diagnostic Features
Some diagnostic features include:
- Grandiose Sense of Self-Importance: Exaggerating achievements, expecting recognition.
- Preoccupation with Fantasies: Dreams of unlimited success, power, or ideal love.
- Belief in Being Special: Insisting on association with high-status individuals.
- Need for Excessive Admiration: Constant need for validation.
- Sense of Entitlement: Expecting special treatment.
- Exploitative Behavior: Using others for personal gain.
- Lack of Empathy: Difficulty appreciating others’ needs.
- Envy of Others: Or belief that others envy them.
- Arrogant Behaviors: Condescending or patronizing attitude.
Causes and Risk Factors
Some causes include:
- Genetic Vulnerability: Traits like low empathy may be heritable.
- Early Childhood Environment: Two main theories: overvaluation model: excessive praise leads to inflated self-view, and neglect/criticism model: narcissism as a defense against shame
- Cultural Influences: Cultures valuing competition and self-promotion may reinforce narcissistic traits.
- Parenting Styles: Overindulgence, excessive admiration, or inconsistent caregiving.
Treatment
NPD is difficult to treat due to lack of insight.
- Schema Therapy: Addresses schemas of entitlement, defectiveness, and admiration-seeking.
- Psychodynamic Therapy: Explores childhood roots of vulnerability.
- CBT: Challenges grandiose beliefs and enhances empathy. Medication is only used for comorbid anxiety or depression.
Conclusion
Cluster-B personality disorders represent complex and deeply ingrained patterns of emotional dysregulation, impulsivity, attention-seeking, and interpersonal instability. While they vary in presentation—ranging from antisocial behavior and aggression to dramatic emotionality or grandiose self-importance—they share core features of emotional intensity and erratic behavior. Treatment success depends heavily on motivation, therapeutic alliance, and the individual’s willingness to challenge long-standing patterns of behavior. Advances in psychotherapy, especially DBT and schema therapy, have significantly improved outcomes, particularly for individuals with BPD.
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Barlow, D. H., & Durand, V. M. (2005). Abnormal Psychology (4th ed.). Brooks/Cole.
Butcher, J. N., Hooley, J. M., & Mineka, S. (2014). Abnormal Psychology (15th ed.). Pearson.
Carson, R. C., Butcher, J. N., & Mineka, S. (2007). Abnormal Psychology (13th ed.). Pearson.
Nevid, J. S., Rathus, S. A., & Greene, B. (2014). Abnormal Psychology (9th ed.). Pearson.
Sarason, I. G., & Sarason, R. B. (2002). Abnormal Psychology (10th ed.). Pearson.
Sue, D., Sue, D. W., & Sue, S. (2006). Understanding Abnormal Behavior (8th ed.). Houghton Mifflin.
Niwlikar, B. A. (2025, December 8). Cluster-B Personality Disorders: Features, 4 Important Types, Causes, and Treatment. Careershodh. https://www.careershodh.com/cluster-b-personality-disorders/
