Introduction
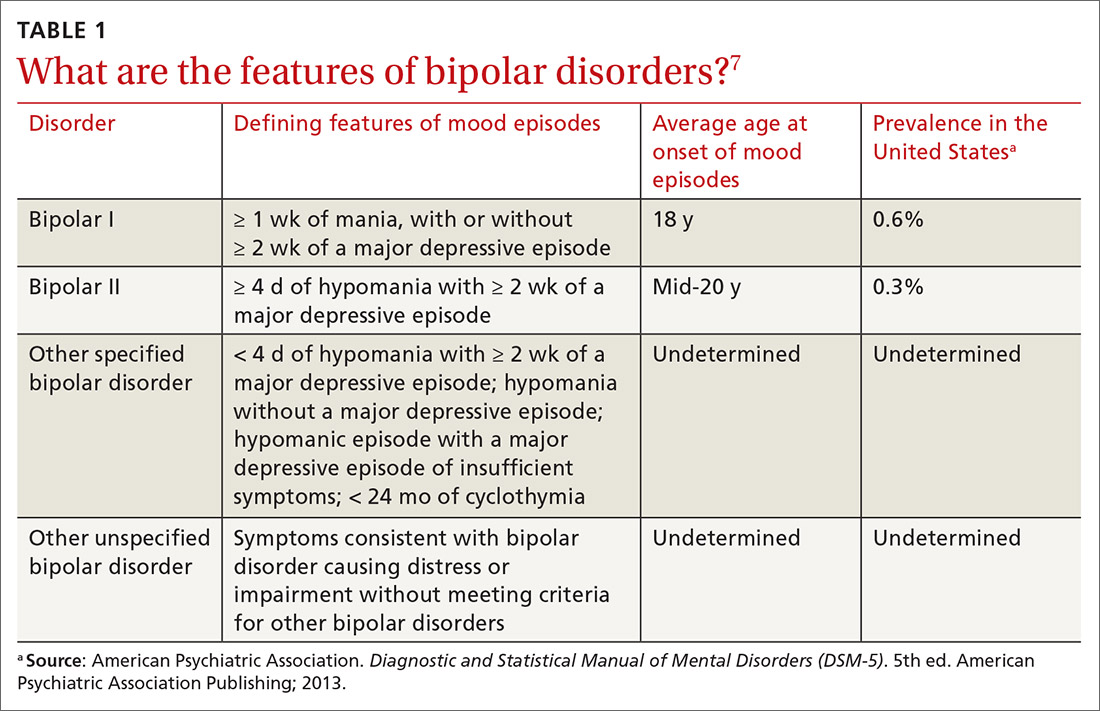
Bipolar disorders are severe mood disorders characterized by alternating episodes of mania or hypomania and depression. They are chronic, recurrent conditions that significantly impair functioning, relationships, and quality of life. According to the DSM-5 (APA, 2013), bipolar disorders include Bipolar I Disorder, Bipolar II Disorder, and Cyclothymic Disorder. Historically, Dysthymic Disorder (now reclassified under Persistent Depressive Disorder in DSM-5) is often discussed in the context of mood spectrum conditions due to its chronic depressive presentation (Butcher, Mineka, & Hooley, 2014).

Bipolar Disorders
In addition, suicide represents a major concern in bipolar disorders, with significantly elevated rates compared to the general population.
1. Bipolar I Disorder
Bipolar I Disorder is characterized by at least one manic episode, often alternating with depressive episodes. Mania involves elevated, expansive, or irritable mood with increased goal-directed activity, lasting at least one week (APA, 2013).
Diagnostic Criteria
DSM-5 criteria for a manic episode include:
- Mood disturbance: Abnormally elevated, expansive, or irritable mood.
- Duration: At least one week (or any duration if hospitalization is required).
- Symptoms: At least three of the following (four if mood is irritable):
- Inflated self-esteem or grandiosity.
- Decreased need for sleep.
- Increased talkativeness or pressured speech.
- Flight of ideas or racing thoughts.
- Distractibility.
- Increased goal-directed activity or psychomotor agitation.
- Excessive involvement in risky activities.
The disturbance must cause marked impairment, require hospitalization, or include psychotic features (APA, 2013; Comer, 2007).
Etiology
- Genetics: Strong hereditary component; twin studies indicate up to 80% heritability.
- Neurobiology: Dysregulation of dopamine and norepinephrine systems; abnormalities in the amygdala and prefrontal cortex.
- Psychosocial factors: Stressful life events, sleep disruptions, and interpersonal conflicts may trigger episodes (Carson et al., 2007; Andrew, 2011).
Treatment
- Mood stabilizers: Lithium remains the gold standard.
- Anticonvulsants: Valproate, carbamazepine.
- Atypical antipsychotics: Quetiapine, olanzapine.
- Psychotherapy: CBT, Interpersonal and Social Rhythm Therapy (IPSRT).
- Psychoeducation: For patients and families to enhance adherence and prevent relapse (Butcher et al., 2014; Barlow & Durand, 2005).
2. Bipolar II Disorder
Bipolar II Disorder is characterized by at least one hypomanic episode and one major depressive episode, but no full manic episodes (APA, 2013). Hypomania is similar to mania but less severe and does not cause marked impairment.
Diagnostic Criteria
- Hypomanic episode: Elevated, expansive, or irritable mood lasting at least four consecutive days.
- At least three additional manic symptoms (e.g., decreased need for sleep, pressured speech, increased activity).
- Observable by others but not severe enough to require hospitalization or cause psychosis.
- Presence of major depressive episodes with classic symptoms (sadness, anhedonia, hopelessness, cognitive impairment).
Etiology
- Genetic risk: Shared genetic basis with Bipolar I.
- Neurotransmitter dysregulation: Particularly involving serotonin and dopamine.
- Stress-diathesis model: Stressful life events precipitate episodes in vulnerable individuals (Alloy, Riskind, & Manos, 2005).
Treatment
- Mood stabilizers: Lithium, lamotrigine (especially effective for depressive episodes).
- Antidepressants: Used cautiously, as they may induce hypomania.
- Psychotherapy: CBT and family therapy improve coping and adherence.
- Lifestyle regulation: Sleep hygiene and stress management are crucial (Andrew, 2011; Nevid, Rathus, & Greene, 2014).
Bipolar Disorders
3. Cyclothymic Disorder
Cyclothymic Disorder is a chronic mood disturbance involving fluctuations between hypomanic symptoms and depressive symptoms that do not meet full criteria for major episodes. Symptoms persist for at least two years in adults (one year in children/adolescents) (APA, 2013).
Diagnostic Criteria
- Numerous periods of hypomanic and depressive symptoms for at least two years.
- Symptoms present at least half the time and not absent for more than two months.
- No history of full manic, hypomanic, or major depressive episodes.
- Causes distress or impairment (Comer, 2007; Carson et al., 2007).
Etiology
- Genetic predisposition: Family history of bipolar disorders.
- Temperament: Emotional instability and high sensitivity.
- Stressors: Chronic stress or unstable environments exacerbate symptoms (Butcher et al., 2014).
Treatment
- Mood stabilizers: Lithium, valproate.
- Psychotherapy: CBT, supportive therapy.
- Monitoring: Risk of progression to Bipolar I or II disorder requires long-term management (Barlow & Durand, 2005).
Bipolar Disorders
4. Dysthymic Disorder (Persistent Depressive Disorder)
Although now subsumed under Persistent Depressive Disorder (PDD) in DSM-5, Dysthymic Disorder historically referred to chronic, low-grade depression. Its relevance to bipolar spectrum discussions arises from its overlap with cyclothymic mood instability (APA, 2013).
Clinical Features
- Chronic depressed mood lasting two or more years.
- At least two additional symptoms: hopelessness, fatigue, low self-esteem, or poor concentration.
- Functional impairment though less severe than MDD (Nevid et al., 2014).
Treatment
- Antidepressants combined with psychotherapy.
- Lifestyle interventions to improve resilience.
- Long-term management to prevent worsening into MDD or bipolar depression (Sue, Sue, & Sue, 2006).
Read More: Suicide
Suicide
Suicide is the intentional act of taking one’s own life. It is a major global health concern and disproportionately affects individuals with mood disorders, particularly bipolar disorder and major depression (WHO, 1992).
Types of Suicide
- Egoistic suicide: Lack of social integration and isolation.
- Altruistic suicide: Perceived benefit to others (e.g., self-sacrifice).
- Anomic suicide: Triggered by social or economic upheaval.
- Fatalistic suicide: Arising from oppressive circumstances or hopelessness (Durkheim’s classification; Sarason & Sarason, 2002).
Causes of Suicide
- Psychiatric disorders: Bipolar disorder, depression, schizophrenia.
- Neurobiological factors: Low serotonin levels linked to impulsivity.
- Psychological factors: Hopelessness, cognitive rigidity, impaired problem-solving.
- Environmental stressors: Trauma, loss, financial problems, relationship difficulties.
- Cultural influences: Stigma, access to lethal means, and lack of social support (Butcher et al., 2014; Nolen-Hoeksema, 2004).
Treatment and Prevention
- Crisis intervention: Hotlines, emergency care, and hospitalization when risk is acute.
- Psychotherapy:
- CBT for suicidal ideation.
- Dialectical Behavior Therapy (DBT) for emotional regulation.
- Pharmacotherapy: Antidepressants, lithium (notably reduces suicide risk in bipolar patients).
- Social interventions: Strengthening family support, community awareness.
- Restricting access to means: Reducing availability of firearms, pesticides, or medications (Andrew, 2011; Sue et al., 2006).
Conclusion
Bipolar disorders represent a spectrum of severe mood dysregulations ranging from full manic episodes in Bipolar I to chronic mood instability in Cyclothymic Disorder. Their biological underpinnings, coupled with psychosocial influences, highlight the need for integrated treatment approaches involving mood stabilizers, psychotherapy, and psychoeducation. Suicide, closely linked to these disorders, underscores the urgency of early detection, effective intervention, and prevention strategies. With timely, evidence-based care, outcomes for individuals with bipolar disorders and suicidal tendencies can be significantly improved.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
Alloy, L. B., Riskind, J. H., & Manos, M. J. (2005). Abnormal psychology: Current perspectives (9th ed.). New Delhi, India: Tata McGraw-Hill.
Andrew, M. (2011). Clinical psychology: Science, practice, and culture (2nd ed.). Sage Publications.
Barlow, D. H., & Durand, V. M. (2005). Abnormal psychology (4th ed.). Pacific Grove, CA: Books/Cole.
Butcher, J. N., Mineka, S., & Hooley, J. M. (2014). Abnormal psychology (15th ed.). Delhi: Dorling Kindersley (India) Pvt. Ltd.
Carson, R. C., Butcher, J. N., Mineka, S., & Hooley, J. M. (2007). Abnormal psychology (13th ed.). India: Pearson Education.
Comer, R. J. (2007). Abnormal psychology (6th ed.). New York: Worth Publishers.
Nevid, J. S., Rathus, S. A., & Greene, B. (2014). Abnormal psychology (9th ed.). Pearson Education.
Nolen-Hoeksema, S. (2004). Abnormal psychology (3rd ed.). New York, NY: McGraw Hill.
Sarason, I. G., & Sarason, R. B. (2002). Abnormal psychology: The problem of maladaptive behavior (10th ed.). Delhi: Pearson Education.
Sue, D., Sue, D. W., & Sue, S. (2006). Abnormal behavior (8th ed.). Houghton Mifflin Company.
World Health Organization. (1992). The ICD-10 classification of mental and behavioural disorders: Clinical description and diagnostic guidelines. Delhi: Oxford University Press.
Niwlikar, B. A. (2025, October 3). 4 Important Bipolar Disorders: Bipolar I, Bipolar II, Cyclothymic Disorder, Dysthymic Disorder, and Suicide. Careershodh. https://www.careershodh.com/bipolar-disorders/
