Introduction
Ethical considerations lies at the heart of psychotherapy. Every therapeutic encounter involves a relationship built on trust, respect, and professional responsibility. The ethical dimension of psychotherapy extends beyond adherence to codes of conduct—it encompasses a moral commitment to safeguard clients’ welfare, promote autonomy, and maintain professional integrity (Gelso & Williams, 2022). Ethical considerations are not static rules but evolving principles that guide therapists through complex human situations shaped by culture, power, and emotion.
Ethics in Psychotherapy
As psychotherapeutic modalities expand and diversify, ethical challenges become more nuanced. Issues such as confidentiality, informed consent, competence, boundaries, dual relationships, and cultural sensitivity demand thoughtful reflection and judgment.
Read More: Projective Techniques
Foundations of Ethical Practice in Psychotherapy
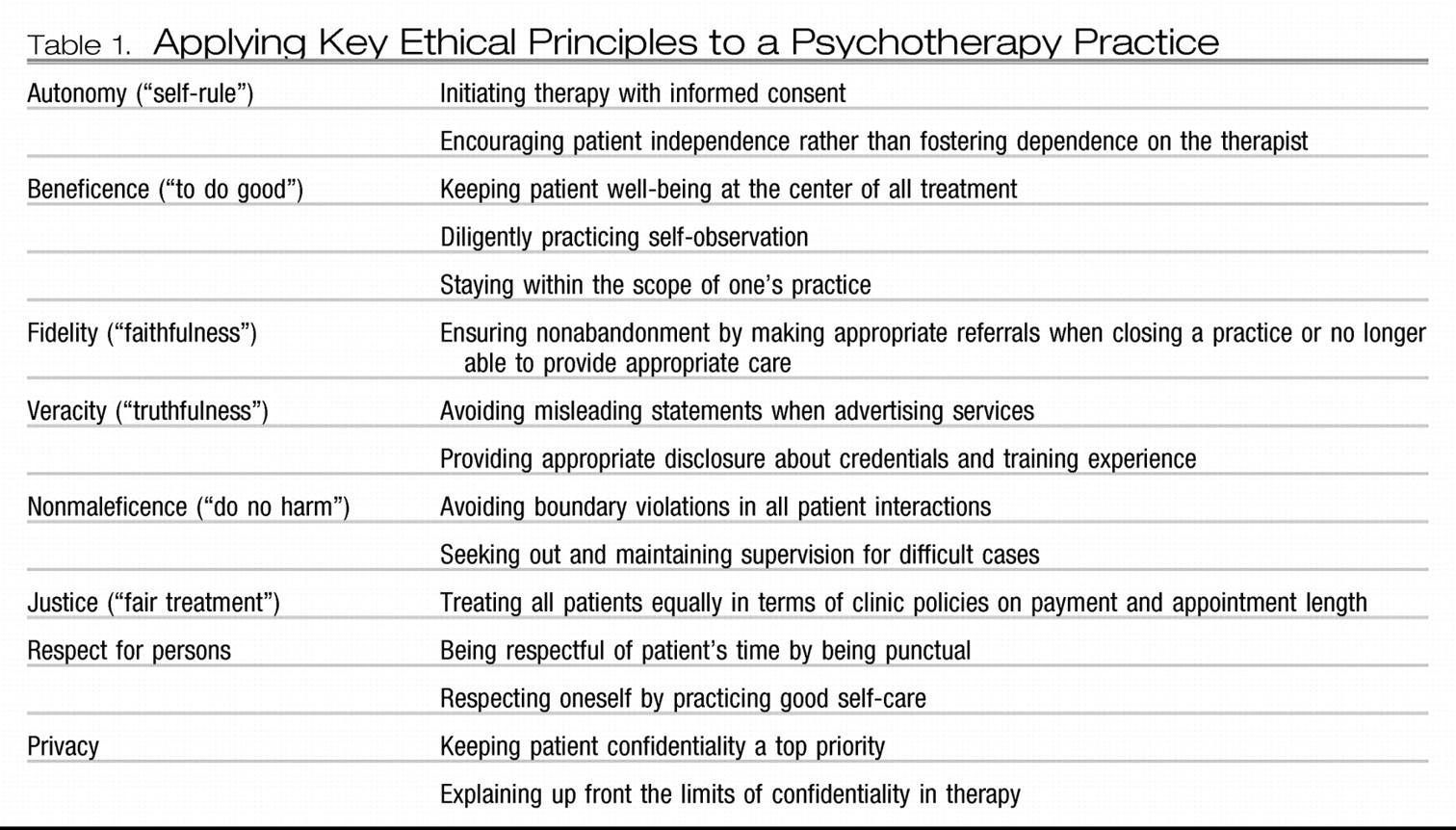
Ethical psychotherapy is guided by professional codes—such as those of the American Psychological Association (APA) and the British Association for Counselling and Psychotherapy (BACP)—that define standards for professional conduct. However, as Gelso and Williams (2022) note, ethics in counseling psychology extend beyond compliance; they involve the cultivation of ethical awareness and personal values consistent with the principles of beneficence, nonmaleficence, autonomy, justice, and fidelity.
The principle of beneficence refers to promoting clients’ well-being, while nonmaleficence mandates avoiding harm. Autonomy respects the client’s right to self-determination, justice emphasizes fairness and equality in access to services, and fidelity entails trustworthiness in maintaining confidentiality and honoring commitments (Feltham & Horton, 2006). These principles serve as the moral compass for navigating dilemmas that arise in therapy.
Gelso and Fretz (1995) emphasize that ethical behavior in counseling psychology is not purely rule-based but relational and contextual. The therapeutic relationship itself is an ethical space that requires honesty, empathy, and accountability. Decisions about intervention, self-disclosure, or termination involve moral reflection and professional discernment grounded in both ethical standards and psychological theory.
1. Confidentiality and Its Limits
Confidentiality forms the cornerstone of the therapeutic alliance, enabling clients to disclose personal material without fear of exposure. Clients must be assured that their disclosures remain private except under legally or ethically justified circumstances (Gelso & Williams, 2022). Confidentiality fosters trust and psychological safety, yet its boundaries are not absolute.
Exceptions arise in situations involving potential harm to self or others, child abuse, or court orders. The ethical challenge lies in balancing the duty to protect client privacy with broader societal responsibilities. According to Feltham and Horton (2006), the therapist’s obligation to prevent harm may sometimes supersede confidentiality, but such breaches must be executed with transparency and minimal intrusion.
In group and family therapies, confidentiality becomes more complex. Corey (2008) notes that therapists cannot guarantee privacy among multiple participants and must emphasize mutual respect and shared responsibility for maintaining confidentiality. Similarly, systemic therapists encounter dilemmas when individual disclosures affect other family members. Ethical practice requires clear contracting and discussion of confidentiality limits at the outset of therapy (Prochaska & Norcross, 2007).
2. Informed Consent and Client Autonomy
Informed consent reflects respect for the client’s autonomy and right to make voluntary, informed decisions about therapy. It requires that clients understand the goals, methods, potential risks, benefits, and limits of confidentiality before engaging in treatment (Capuzzi & Gross, 2008). The process is ongoing rather than a one-time administrative act—it evolves as therapy progresses and as new interventions or risks emerge.
Gelso and Williams (2022) emphasize that informed consent embodies both ethical and legal principles. Ethically, it supports collaboration and transparency; legally, it protects clients and therapists from misunderstandings or coercion. For example, in cognitive-behavioral therapy, clients are often active participants in setting goals and selecting interventions, reinforcing autonomy.
In certain contexts, such as with minors or individuals with impaired decision-making capacity, obtaining consent involves additional ethical sensitivity. Verma (1990) highlights that with children and adolescents, therapists must balance parental rights with the young client’s right to privacy and participation. The therapist’s ethical role is to ensure understanding appropriate to developmental level while advocating for the client’s best interests.
3. Competence and Professional Boundaries
Therapists are ethically obligated to practice within their areas of competence, defined by education, training, supervision, and professional experience. Incompetent or unqualified practice may result in harm, violating the principles of beneficence and nonmaleficence (Feltham & Horton, 2006). Maintaining competence requires continual professional development, supervision, and awareness of one’s limitations.
Gelso and Williams (2022) stress that competence is not merely technical but personal—it includes self-awareness, emotional regulation, and the ability to manage countertransference. Therapists must monitor their own reactions and biases that could distort therapeutic judgment. Similarly, supervision and peer consultation serve as ethical safeguards, ensuring accountability and reflective practice (Woolfe & Dryden, 1996).
Boundary management is another crucial ethical concern. Boundaries delineate the professional nature of the therapeutic relationship and protect clients from exploitation or confusion. Boundary violations—such as dual relationships, inappropriate self-disclosure, or sexual involvement—erode trust and cause harm (Feltham & Horton, 2006). While flexibility in boundaries may be therapeutically appropriate in certain cultural or community contexts, therapists must evaluate the intent, potential impact, and power dynamics involved.
4. Dual Relationships and Power Dynamics
Dual relationships occur when a therapist assumes multiple roles with a client—such as being both a counselor and a business associate, friend, or supervisor. Although some dual roles are unavoidable, especially in small or rural communities, they carry risks of exploitation, impaired judgment, and loss of objectivity (Gelso & Fretz, 1995).
The ethical challenge lies in assessing whether a dual relationship enhances or undermines therapeutic effectiveness. Prochaska and Norcross (2007) argue that transparency, informed consent, and consultation are critical when navigating these situations. Therapists should avoid any relationship that may compromise professional boundaries or client welfare.
Power imbalance is inherent in psychotherapy—the therapist possesses knowledge, authority, and access to the client’s vulnerabilities. Ethical awareness requires therapists to use this power responsibly, promoting empowerment rather than dependency (Nelson-Jones, 2009). Humanistic and existential modalities, for example, emphasize equality and authenticity, seeking to reduce hierarchical dynamics by positioning the therapist as a facilitator rather than an expert (Feltham & Horton, 2006).
5. Cultural and Contextual Ethics
Ethical practice cannot be divorced from cultural context. Gelso and Williams (2022) highlight that multicultural competence is an ethical imperative in counseling psychology. Therapists must understand how culture, ethnicity, gender, religion, and socioeconomic status shape clients’ experiences, values, and expressions of distress. Failure to consider cultural factors may lead to misdiagnosis, bias, or cultural imposition.
Veereshwar (2002) and Ajaya (1989) emphasize that psychotherapy must align with indigenous philosophies and healing traditions when practiced in non-Western contexts. For instance, yoga-based psychotherapy (Rama, Ballentine, & Ajaya, 1976) integrates mind-body-spirit awareness consistent with Eastern ethical principles of balance and compassion. Similarly, Watts (1973) argues that psychotherapy should not be confined to Western individualism but should embrace global perspectives on consciousness and healing.
Ethical sensitivity also involves respecting cultural variations in communication, family roles, and power hierarchies. What may be considered a boundary violation in one culture—such as physical touch or therapist self-disclosure—may be seen as caring in another. Therapists must therefore apply ethical principles flexibly, informed by cultural understanding and client collaboration (Feltham & Horton, 2006).
Research, Evidence, and Ethical Responsibility
Ethical psychotherapy also entails commitment to evidence-based practice and scientific integrity. Therapists must rely on empirically supported interventions and avoid untested or potentially harmful techniques (Capuzzi & Gross, 2008). Research ethics demand informed consent, confidentiality, and protection from harm for participants.
Gelso and Williams (2022) emphasize that ethical decision-making in practice and research is an ongoing process requiring critical reflection and sensitivity to contextual variables. Therapists must weigh empirical evidence alongside clinical expertise and client preferences—the tripartite model of evidence-based practice. Neglecting scientific rigor or overreliance on intuition may lead to ethical lapses.
Moreover, ethical responsibility includes accurate record-keeping, truthful representation of credentials, and avoidance of plagiarism or misrepresentation in academic and clinical documentation (Feltham & Horton, 2006). Professional honesty sustains trust not only with clients but also within the broader scientific and clinical community.
Technology, Confidentiality, and Emerging Ethical Challenges
With the advent of digital technology and telepsychology, new ethical challenges have emerged. Online counseling raises questions about confidentiality, data security, and informed consent across jurisdictions. Therapists must ensure secure communication platforms and clarify risks related to privacy breaches (Gelso & Williams, 2022).
Capuzzi and Gross (2008) suggest that while technology expands access to therapy, it also demands heightened vigilance regarding professional boundaries and emergency procedures. The lack of physical presence may complicate assessment of risk or crisis situations. Ethical telepractice involves clear communication, informed consent specific to digital contexts, and adherence to licensing laws across regions.
Ethical Decision-Making Models
Ethical dilemmas in psychotherapy often present conflicts between competing values. Structured decision-making models help therapists navigate such complexities systematically. Prochaska and Norcross (2007) and Feltham and Horton (2006) outline stepwise models that involve identifying the problem, consulting ethical codes, considering possible courses of action, evaluating consequences, and documenting decisions.

Ethical Decision Making
Supervision and consultation are integral to ethical decision-making, offering diverse perspectives and reducing individual bias. Gelso and Williams (2022) note that self-reflective awareness—recognizing one’s motives, countertransference, and moral intuitions—is essential for ethical maturity. Ultimately, ethical decision-making blends professional standards with empathy and moral reasoning, ensuring client welfare remains central.

Ethical Decision Making
Conclusion
Ethical considerations in psychotherapy encompass far more than rule compliance—they represent the lived expression of professional integrity, respect, and compassion. From confidentiality and informed consent to cultural sensitivity and technological ethics, therapists must navigate complex moral terrains guided by core principles of beneficence, nonmaleficence, autonomy, justice, and fidelity.
As Gelso and Williams (2022) affirm, ethical practice is inseparable from the quality of the therapeutic relationship and the therapist’s self-awareness. Each therapeutic encounter calls for humility, reflection, and commitment to clients’ welfare. The evolving landscape of psychotherapy—shaped by cultural diversity, digital innovation, and global interconnectedness—demands renewed ethical vigilance and adaptability. By integrating ethical reflection into daily practice, psychotherapists honor the profession’s ultimate purpose: to promote healing, dignity, and human flourishing.
References
Ajaya, S. (1989). Psychotherapy: East and West. Hinsdale, PA: Himalayan International Institute.
Capuzzi, D., & Gross, D. R. (2008). Counseling and psychotherapy: Theories and interventions (4th ed.). Pearson Education India.
Corey, G. (2008). Theory and practice of group counseling. Belmont, CA: Thomson Brooks/Cole.
Feltham, C., & Horton, I. E. (Eds.). (2006). The Sage handbook of counselling and psychotherapy (2nd ed.). London: Sage Publications.
Gelso, C. J., & Fretz, B. R. (1995). Counselling psychology. Bangalore: Prism Books Pvt. Ltd.
Gelso, C. J., & Williams, E. N. (2022). Counseling psychology. Washington, DC: American Psychological Association.
Nelson-Jones, R. (2009). Theory and practice of counselling and therapy (4th ed.). London: Sage Publications.
Prochaska, J. O., & Norcross, J. C. (2007). Systems of psychotherapy: A transtheoretical analysis (6th ed.). Belmont, CA: Thomson Brooks/Cole.
Rama, S., Ballentine, R., & Ajaya, S. (1976). Yoga and psychotherapy. Hinsdale, PA: Himalayan International Institute.
Veereshwar, P. (2002). Indian systems of psychotherapy. Delhi: Kalpaz Publications.
Verma, L. (1990). The management of children with emotional and behavioral difficulties. London: Routledge.
Watts, A. W. (1973). Psychotherapy: East and West. London: Penguin Books.
Woolfe, R., & Dryden, W. (Eds.). (1996). Handbook of counseling psychology. New Delhi: Sage Publications.
Niwlikar, B. A. (2025, November 3). 5 Important Ethical Considerations in Psychotherapies. Careershodh. https://www.careershodh.com/ethical-considerations-in-psychotherapies/
