Introduction
Depressive disorders constitute a group of psychiatric conditions characterized by persistent disturbances in mood, cognition, and behavior. They represent some of the most prevalent mental health disorders globally, significantly impairing quality of life and functioning.

Depressive Disorders
According to the DSM-5 (APA, 2013), depressive disorders include Major Depressive Disorder (MDD), Disruptive Mood Dysregulation Disorder (DMDD), Persistent Depressive Disorder (PDD, formerly Dysthymia), and Premenstrual Dysphoric Disorder (PMDD). Each disorder presents unique diagnostic features, but all share a common core of depressed mood, anhedonia, and impaired functioning.
Read More: DSM vs ICD
1. Major Depressive Disorder (MDD)
Major Depressive Disorder is the most recognized depressive disorder, marked by at least one episode of severe depression lasting a minimum of two weeks. Symptoms include persistent sadness, loss of interest in pleasurable activities, cognitive impairments, and somatic complaints (APA, 2013; Barlow & Durand, 2005).
Major Depressive Disorder
Symptoms
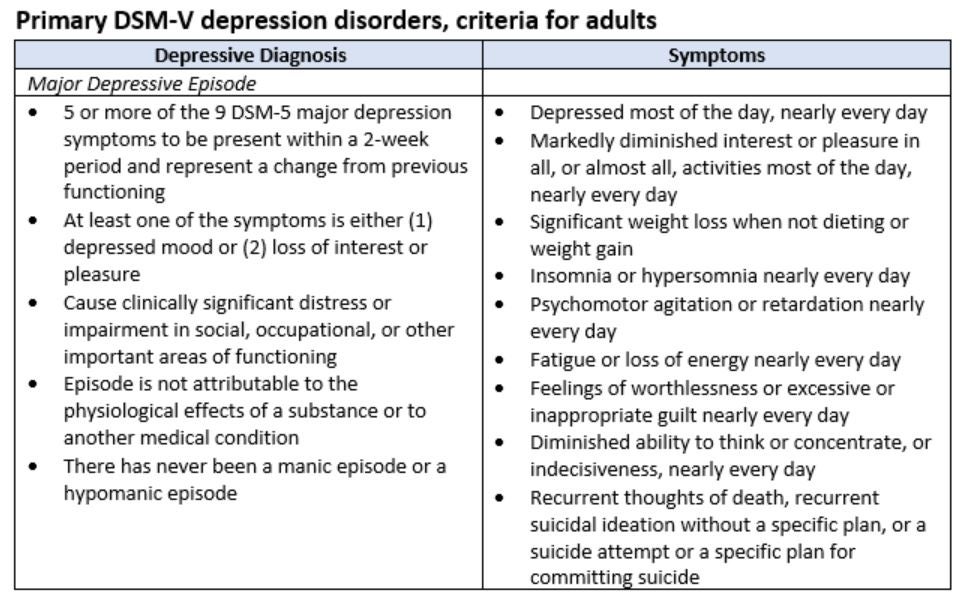
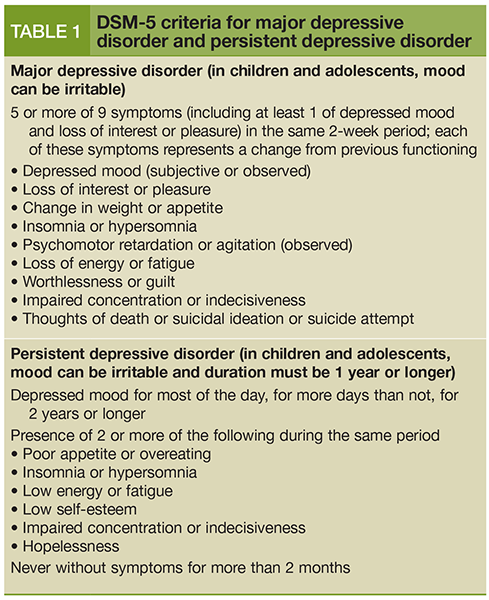
DSM-5 diagnostic criteria for MDD require five or more symptoms during the same 2-week period, including depressed mood or loss of interest. Symptoms include:
- Depressed mood most of the day.
- Diminished interest or pleasure in activities.
- Significant weight loss or gain, or appetite changes.
- Insomnia or hypersomnia.
- Psychomotor agitation or retardation.
- Fatigue or loss of energy.
- Feelings of worthlessness or excessive guilt.
- Diminished concentration or indecisiveness.
- Recurrent thoughts of death or suicidal ideation (APA, 2013; Butcher, Mineka, & Hooley, 2014).
Symptoms must cause significant impairment and not be attributable to substances or medical conditions.
Etiology
MDD arises from an interaction of biological, psychological, and environmental factors:
- Biological: Neurotransmitter imbalances (serotonin, norepinephrine, dopamine), genetic predisposition, and HPA-axis dysregulation (Carson et al., 2007).
- Psychological: Cognitive distortions, maladaptive beliefs, and learned helplessness (Seligman’s theory).
- Environmental: Stressful life events, interpersonal loss, childhood trauma, and socioeconomic disadvantage (Andrew, 2011; Alloy, Riskind, & Manos, 2005).
Treatment
- Pharmacotherapy: SSRIs, SNRIs, tricyclic antidepressants, and MAOIs.
- Psychotherapy: Cognitive Behavioral Therapy (CBT), Interpersonal Therapy (IPT).
- Electroconvulsive Therapy (ECT): Effective in treatment-resistant depression.
- Lifestyle interventions: Exercise, sleep regulation, and stress management (Barlow & Durand, 2005; Nevid, Rathus, & Greene, 2014).
3. Disruptive Mood Dysregulation Disorder (DMDD)
Introduced in DSM-5, DMDD is a childhood-onset disorder characterized by severe temper outbursts and persistent irritability, distinct from pediatric bipolar disorder. It aims to address overdiagnosis of bipolar disorder in children (APA, 2013).
Symptoms
Diagnostic features include:
- Severe recurrent temper outbursts (verbal or behavioral).
- Outbursts disproportionate to the situation.
- Occurrence at least 3 times per week.
- Persistent irritability between outbursts.
- Duration: at least 12 months, with symptoms present in two or more settings.
- Diagnosis between ages 6 and 18 years (APA, 2013; Comer, 2007).
Etiology
- Biological factors: Abnormalities in brain circuits regulating mood and impulse control.
- Environmental factors: Chaotic home environments, inconsistent parenting, or trauma.
- Genetic predisposition: Family history of mood and anxiety disorders (Butcher et al., 2014).
Treatment
- Psychotherapy: Parent training, CBT for emotional regulation.
- Medication: Stimulants, antidepressants, or atypical antipsychotics when necessary.
- Family-focused interventions: Improving parenting strategies and family communication (Andrew, 2011).
4. Persistent Depressive Disorder (PDD)
Formerly called Dysthymia, PDD is characterized by chronic low-grade depression lasting at least two years in adults or one year in children/adolescents (APA, 2013).
Persistent Depressive Disorder
Symptoms
Key features include:
- Depressed mood most of the day, more days than not.
- Presence of at least two additional symptoms:
- Poor appetite or overeating.
- Insomnia or hypersomnia.
- Low energy or fatigue.
- Low self-esteem.
- Poor concentration or difficulty making decisions.
- Feelings of hopelessness.
Symptoms are milder than MDD but more chronic (Carson et al., 2007; Sue, Sue, & Sue, 2006).
Etiology
- Neurobiological: Chronic dysregulation of neurotransmitters.
- Cognitive-behavioral: Persistent maladaptive thinking patterns.
- Environmental: Ongoing stress, chronic illness, or adverse childhood experiences.
- Genetic vulnerability: Family history of depression increases risk (Alloy et al., 2005).
Treatment
- Psychotherapy: CBT, Dialectical Behavior Therapy (DBT), and IPT.
- Pharmacotherapy: Antidepressants, often in combination with therapy.
- Lifestyle management: Long-term coping strategies for stress resilience (Barlow & Durand, 2005).
5. Premenstrual Dysphoric Disorder (PMDD)
PMDD is a severe form of premenstrual syndrome marked by mood disturbances, irritability, and somatic symptoms that impair functioning. It occurs in the luteal phase of the menstrual cycle and resolves after menstruation (APA, 2013).
Symptoms
DSM-5 requires five or more symptoms, with at least one being mood-related:
- Affective lability (mood swings).
- Irritability or anger.
- Depressed mood or hopelessness.
- Anxiety or tension.
- Physical symptoms: bloating, breast tenderness, joint pain.
- Decreased interest in activities, difficulty concentrating, fatigue, changes in sleep or appetite (Butcher et al., 2014; Nevid et al., 2014).
Etiology
- Hormonal fluctuations: Sensitivity to changes in estrogen and progesterone.
- Serotonergic dysfunction: Low serotonin linked to mood disturbances.
- Psychosocial stressors: Interpersonal conflict, poor coping skills (Andrew, 2011; Alloy et al., 2005).
Treatment
- Pharmacotherapy: SSRIs (effective in luteal-phase dosing), oral contraceptives.
- Lifestyle: Exercise, diet regulation, and stress reduction.
- Psychotherapy: CBT to manage mood symptoms.
- Nutritional interventions: Calcium and vitamin B6 supplementation (Barlow & Durand, 2005).
Conclusion
Depressive disorders encompass diverse conditions ranging from severe episodes of major depression to chronic low-grade symptoms and cyclical mood changes. While they differ in onset, duration, and severity, all profoundly impair emotional and social functioning. Advances in neurobiological research and psychotherapeutic interventions have improved outcomes. Effective management often requires an integrative approach, combining pharmacological, psychological, and lifestyle interventions. Early recognition and treatment remain essential to prevent chronicity and enhance quality of life.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
Alloy, L. B., Riskind, J. H., & Manos, M. J. (2005). Abnormal psychology: Current perspectives (9th ed.). New Delhi, India: Tata McGraw-Hill.
Andrew, M. (2011). Clinical psychology: Science, practice, and culture (2nd ed.). Sage Publications.
Barlow, D. H., & Durand, V. M. (2005). Abnormal psychology (4th ed.). Pacific Grove, CA: Books/Cole.
Butcher, J. N., Mineka, S., & Hooley, J. M. (2014). Abnormal psychology (15th ed.). Delhi: Dorling Kindersley (India) Pvt. Ltd.
Carson, R. C., Butcher, J. N., Mineka, S., & Hooley, J. M. (2007). Abnormal psychology (13th ed.). India: Pearson Education.
Comer, R. J. (2007). Abnormal psychology (6th ed.). New York: Worth Publishers.
Nevid, J. S., Rathus, S. A., & Greene, B. (2014). Abnormal psychology (9th ed.). Pearson Education.
Sue, D., Sue, D. W., & Sue, S. (2006). Abnormal behavior (8th ed.). Houghton Mifflin Company.
Niwlikar, B. A. (2025, October 2). 4 Important Depressive Disorders: Diagnostic Criteria, Etiology, and Treatment. Careershodh. https://www.careershodh.com/depressive-disorders/
