Introduction
Personality disorders are enduring, pervasive, and inflexible patterns of thinking, feeling, and behaving that deviate sharply from cultural expectations and lead to significant impairment in interpersonal, occupational, and emotional functioning. Among the DSM-5 (American Psychiatric Association, 2013) classification, Cluster-A personality disorders represent the group traditionally described as odd or eccentric. These disorders share characteristics with schizophrenia-spectrum conditions, especially in terms of cognitive distortions, perceptual abnormalities, and unusual or eccentric behavior. However, unlike psychotic disorders, the symptoms in Cluster-A disorders do not include persistent hallucinations, delusions, or full-blown disorganization.
Cluster-A includes three specific disorders:
- Paranoid Personality Disorder (PPD)
- Schizoid Personality Disorder (SPD)
- Schizotypal Personality Disorder (STPD)
These disorders are often underdiagnosed due to the individuals’ reluctance to seek help and the belief that their perceptions are justified. Cluster-A personality traits typically begin in late childhood or adolescence, remain stable across adulthood, and frequently co-occur with schizophrenia-spectrum disorders in family lines.
Read More: Psychodynamics
General Diagnostic Characteristics of Cluster-A
Although each disorder in this cluster has specific diagnostic criteria, they share certain general features:
1. Social and Interpersonal Detachment
Individuals habitually avoid close relationships, struggle with emotional intimacy, and may prefer isolation. Their interpersonal functioning is significantly affected by mistrust, emotional coldness, or social discomfort.
2. Cognitive and Perceptual Distortions
These distortions are less severe than psychosis, but include:
- Odd beliefs
- Misinterpretation of social cues
- Suspiciousness
- Magical thinking (especially in schizotypal disorder)
3. Eccentric or Unusual Behaviors
Their behavior, mannerisms, or speech may appear peculiar, rigid, or socially inappropriate. This contributes to social rejection, reinforcing isolation.
4. Emotional Restriction
A flattened, limited, or awkward emotional expression is common. They may appear indifferent, aloof, rigid, or awkward in emotional situations.
5. Early Onset and Chronic Course
Symptoms emerge by adolescence or early adulthood and remain stable for decades.
1. Paranoid Personality Disorder (PPD)
Paranoid Personality Disorder is characterized by pervasive distrust and suspiciousness of others, such that their motives are interpreted as malevolent. This pattern exists across contexts and is not limited to occasional episodes.

Paranoid Personality Disorder
Diagnostic Features
According to DSM-5, individuals with PPD:
- Assume others are exploiting, deceiving, or harming them: They habitually suspect that others are intentionally trying to undermine, insult, or sabotage them. Casual remarks are interpreted as threatening.
- Doubt the loyalty and trustworthiness of friends: They believe others harbor hidden motives, leading to chronic mistrust even in close relationships.
- Are reluctant to confide in others: They fear that personal information will be used against them.
- Read hidden insults or threats into neutral events: Benign remarks or facial expressions are perceived as attacks.
- Persistently hold grudges: Even minor slights are remembered and resented for long periods.
- Perceive character attacks and react with anger: They may quickly retaliate with hostility or aggression.
- Unfounded suspicion of infidelity: Often believe without evidence that their partner is unfaithful.
Causes and Risk Factors
- Genetic Vulnerability: PPD is more common among relatives of individuals with schizophrenia and delusional disorder.
- Early Family Environment: Exposure to neglect, harsh criticism, humiliating experiences, or parental hostility contributes to a worldview structured around mistrust.
- Cognitive Biases: Stable maladaptive beliefs such as: “People are dangerous.” “If I am not vigilant, others will take advantage of me.”
- Cultural and Social Factors: Marginalized groups may present hypervigilance due to experiences of oppression; clinicians must differentiate normative mistrust from pathological mistrust.
Treatment Strategies
Individuals with PPD rarely seek treatment voluntarily. When they do, therapy must:
- Establish a Strong Therapeutic Alliance: Trust develops slowly; the therapist must remain professional, consistent, and avoid challenging paranoid beliefs too aggressively.
- Cognitive-Behavioral Therapy (CBT): Used to examine evidence for beliefs, reduce suspicious thoughts, increase flexibility in thinking, and enhance trust-building skills.
- Interpersonal Therapy: Addresses relational styles and communication patterns.
- Medication: Generally not effective unless treating associated symptoms like anxiety or agitation. Low-dose antipsychotics (e.g., risperidone) may help in severe cases.
2. Schizoid Personality Disorder (SPD)
SPD is defined by detachment from social relationships and a restricted range of emotional expression. Individuals appear indifferent to social interactions and seem emotionally cold.

Schizoid Personality Disorder
Diagnostic Features
DSM-5 identifies several core patterns:
- Lack of desire for intimate relationships: They prefer solitary life and rarely pursue romantic or sexual involvement.
- Preference for solitary activities: Jobs or careers involving minimal interaction are preferred.
- Very limited emotional expression: Flattened affect, monotone speech, limited facial expressions.
- Indifference to praise or criticism: They neither seek approval nor feel hurt by rejection.
- Minimal interest in sexual experiences: Lack of strong sexual drive or bonding needs.
- Emotional coldness and detachment: Appearing aloof, absent, or internally distant from the world. SPD is not due to anxiety—it is true disinterest.
Causes and Risk Factors
Some causes and risk factors include:
- Temperamental Factors: Aloof, introverted traits may appear from early childhood.
- Genetic Links: Higher prevalence among relatives of schizophrenia-spectrum patients.
- Early Attachment Problems: Cold, neglectful, or emotionally unavailable parenting leads to internal withdrawal.
- Social Learning: Children who learn to suppress emotions or avoid relationships may internalize these patterns as normal.
Treatment
Treatment is difficult because individuals rarely see their behavior as problematic.
- Supportive Psychotherapy: Focus on social skills, emotional recognition, and small steps toward interpersonal engagement.
- Behavioral Interventions: Training in expressing emotions, increasing social interest, and role-playing interpersonal situations
- Group Therapy: Usually unsuccessful due to discomfort with intimacy, unless gradually structured.
- Medication: Not generally useful unless comorbid depression exists.
3. Schizotypal Personality Disorder (STPD)
Schizotypal Personality Disorder is the most severe disorder in Cluster-A and is considered closest to schizophrenia-spectrum disorders. It presents with social and interpersonal deficits, cognitive or perceptual distortions, and eccentric behaviors.
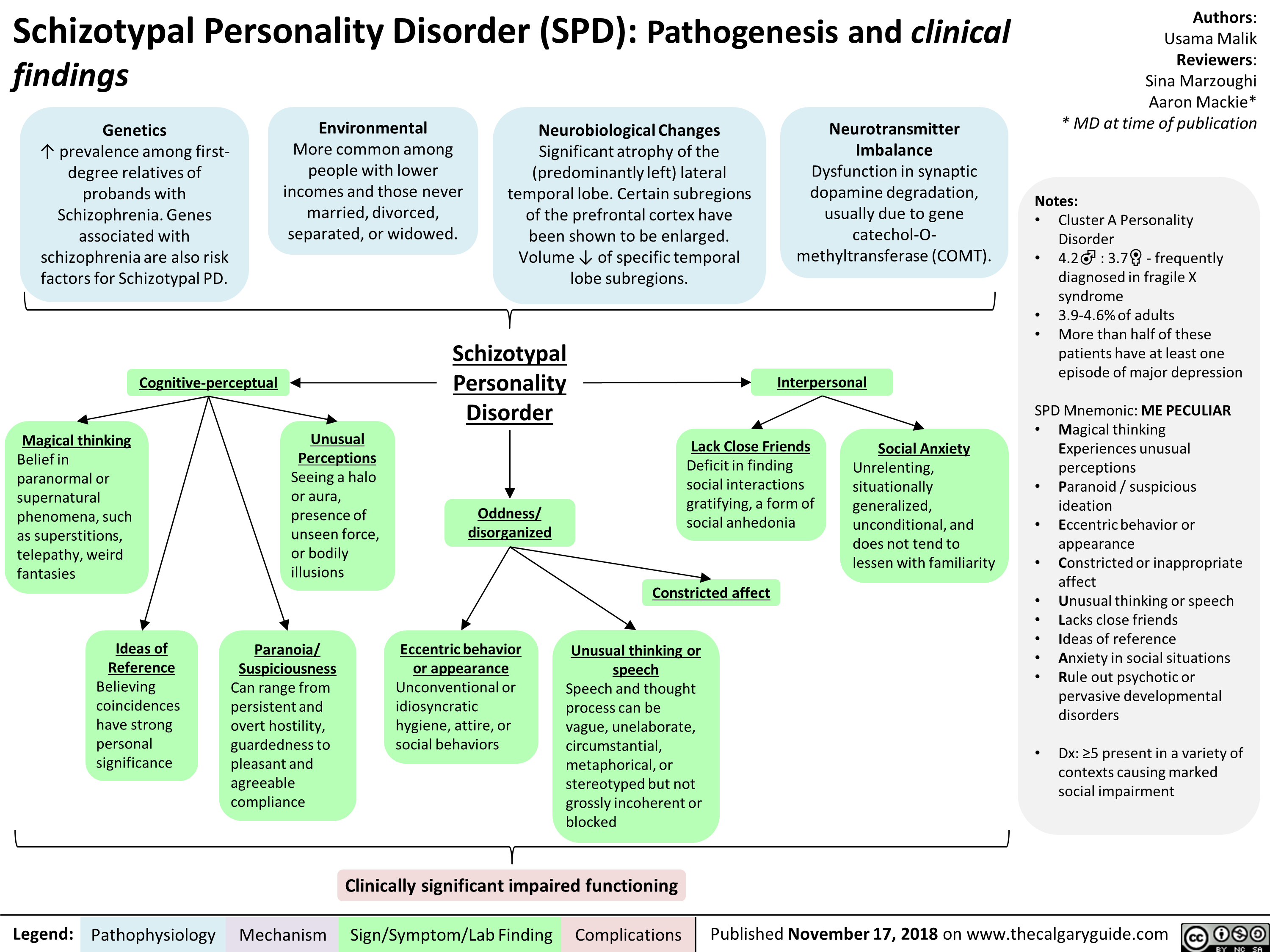
Schizotypal Personality Disorder
Diagnostic Features
Some dignostic features include:
- Ideas of Reference: Belief that unrelated events relate directly to themselves.
- Odd Beliefs or Magical Thinking: Belief in telepathy, sixth sense, superstitions, paranormal phenomena.
- Unusual Perceptual Experiences: Sensing presence of unseen forces, unusual bodily sensations.
- Odd Thinking and Speech: Vague, metaphorical, circumstantial communication.
- Suspiciousness or Paranoid Ideation: Chronic mistrust.
- Inappropriate or Constricted Affect: Emotionally odd reactions, awkward expressions.
- Eccentric Behavior or Appearance: Strange dressing style, peculiar rituals.
- Lack of Close Friends: Not due to anxiety, but discomfort around others.
- Excessive Social Anxiety: Based more on paranoid fear than low self-esteem.
Causes
Some causes for this includes:
- Genetic Factors: Strong link with schizophrenia; first-degree relatives have higher rates of STPD.
- Neurological Abnormalities: impaired working memory, unusual sensory processing, and frontal lobe underactivity
- Childhood Trauma: Neglect, emotional under-stimulation, or inconsistent parenting.
- Cognitive Distortions: Tendency toward odd explanations and misinterpretation of random events.
Treatment
Some treatments include:
- Cognitive-Behavioral Therapy: Addressing distorted beliefs and magical thinking.
- Social Skills Training: Teaching interpersonal norms and communication skills.
- Psychosocial Intervention: Practical guidance for daily functioning.
- Medications: Low-dose antipsychotics help reduce: suspiciousnessunusual perceptual experiences, and anxiety
Conclusion
Cluster-A personality disorders represent complex, enduring patterns of odd thinking, emotional restriction, social detachment, and eccentric behavior. Though distinct from psychosis, their cognitive distortions and interpersonal dysfunction create significant impairment. Treatment remains challenging, especially due to low insight and reluctance to engage, but targeted psychotherapy and occasional medication can reduce distress and improve functioning.
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
Barlow, D. H., & Durand, V. M. (2005). Abnormal Psychology (4th ed.). Brooks/Cole.
Butcher, J. N., Mineka, S., & Hooley, J. M. (2014). Abnormal Psychology (15th ed.). Pearson.
Carson, R. C., Butcher, J. N., & Mineka, S. (2007). Abnormal Psychology (13th ed.). Pearson.
Nevid, J. S., Rathus, S. A., & Greene, B. (2014). Abnormal Psychology (9th ed.). Pearson.
Sue, D., Sue, D. W., & Sue, S. (2006). Understanding Abnormal Behavior (8th ed.). Houghton Mifflin.
Sarason, I. G., & Sarason, R. B. (2002). Abnormal Psychology (10th ed.). Pearson.
Niwlikar, B. A. (2025, December 5). Cluster-A Personality Disorders: Features, 3 Important Types, Causes, and Treatment. Careershodh. https://www.careershodh.com/cluster-a-personality-disorders/
