Introduction
Schizophrenia is a severe, chronic, and heterogeneous psychiatric disorder that profoundly affects thinking, perception, emotion, and behavior. It is considered one of the most disabling mental illnesses due to its pervasive and long-lasting impact on social, occupational, and cognitive functioning. Globally, schizophrenia affects about 1% of the population, and onset typically occurs in late adolescence or early adulthood, with males commonly showing symptoms earlier than females (Butcher, Mineka & Hooley, 2014). Despite advances in treatment, stigma, misunderstanding, and delayed diagnosis remain widespread challenges. Modern research views schizophrenia as a neurodevelopmental disorder associated with complex interactions among biological vulnerability and environmental stress.
Read More: Cognitive Therapy
Definition of Schizophrenia
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) defines schizophrenia as a disorder involving delusions, hallucinations, disorganized speech, disorganized or catatonic behavior, and negative symptoms, persisting for at least six months with at least one month of active symptoms (American Psychiatric Association, 2013). Diagnosis also requires significant impairment in major life areas such as work, interpersonal relationships, and self-care, with symptoms not attributable to substance use or other medical or psychological conditions. This definition highlights schizophrenia not as a single disease but as a syndrome comprised of multiple symptom dimensions.
Phases of Schizophrenia
Schizophrenia typically follows a progressive course with three major phases (Barlow & Durand, 2005):

Schizophrenia
1. Prodromal Phase
The prodromal phase precedes the onset of full psychosis and often spans months or years. It includes subtle personality changes and functional decline such as:
- Increasing social withdrawal and isolation
- Reduced academic or occupational performance
- Disturbances in sleep and concentration
- Growing difficulty in communicating thoughts
- Apathy, lack of interest, and emotional blunting
These symptoms are often mistaken for depression or typical adolescent difficulties, making early detection challenging.
2. Active (Acute) Phase
This phase involves the appearance of overt psychotic symptoms such as:
- Hallucinations (most frequently auditory)
- Delusions
- Thought disorder
- Grossly disorganized or catatonic behavior (APA, 2013)
During this period, individuals may lose touch with reality and behavior may become unpredictable and dangerous, requiring hospitalization for stabilization.
3. Residual Phase
This phase follows treatment of acute symptoms. During this stage:
- Positive symptoms may diminish significantly
- Negative and cognitive symptoms remain prominent
- Social and occupational functioning remains impaired
- Vulnerability to relapse persists (Nevid, Rathus & Greene, 2014)
Residual symptoms can remain lifelong, affecting independence, relationships, and quality of life.
Symptoms of Schizophrenia
Symptoms of schizophrenia are typically categorized into positive, negative, and cognitive symptoms. Each contributes differently to functional disability.
Positive Symptoms
Positive symptoms represent distortions or exaggerations of normal functioning. They are often most noticeable in the active phase and include:
1. Hallucinations: Hallucinations are sensory perceptions occurring without external stimuli. The most common are auditory hallucinations, typically experienced as voices conversing, commenting, or commanding. These voices are often critical, hostile, or threatening (American Psychiatric Association, 2013). Visual, tactile, and olfactory hallucinations occur less frequently and may indicate organic causes.
2. Delusions: Delusions are fixed false beliefs resistant to logical reasoning. Common types include:
- Persecutory delusions: belief that one is being spied on or harmed
- Grandiose delusions: belief in special powers or identity
- Erotomanic delusions: belief that another person is in love with the sufferer
- Referential delusions: belief that events or media messages refer specifically to oneself
- Somatic delusions: belief that the body is diseased or altered (Butcher et al., 2014)
3. Disorganized Speech: Disorganized thought becomes evident through:
- Loose associations (shifting topics with no logical connection)
- Tangentiality (answers unrelated to questions)
- Word salad (incoherent jumble of words)
- Neologisms (made-up words)
Speech disorganization reflects cognitive disruption rather than intentional behavior.
4. Grossly Disorganized or Catatonic Behavior: This includes:
- Unpredictable agitation
- Childlike silliness
- Bizarre postures
- Complete motionlessness
- Waxy flexibility (maintaining awkward positions)
Catatonia may include excessive purposeless movement or rigid immobility (Carson et al., 2007).
Negative Symptoms
Negative symptoms reflect reductions in normal emotional and behavioral functioning and are strongly associated with long-term disability.
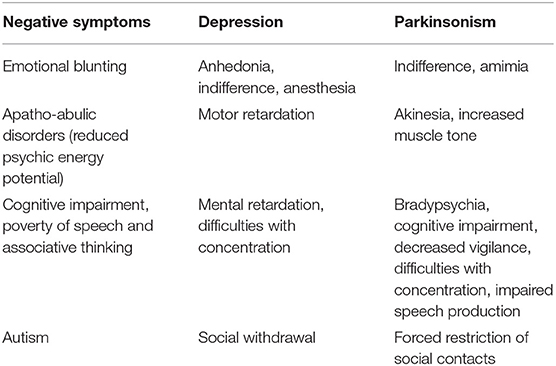
Primary and Secondary Negative Symptoms in Schizophrenia
1. Flat or Blunted Affect: Reduced emotional expression including:
- Monotonous voice
- Minimal facial expressions
- Limited gestures
2. Avolition: Inability to begin or follow through with activities. Individuals may sit for long periods without engaging in purposeful behavior.
3. Alogia: Poverty of speech reflected in brief, sparse replies.
4. Anhedonia: Inability to experience pleasure or interest.
5. Asociality: Disinterest in forming or maintaining interpersonal relationships.
Negative symptoms are often mistaken for depression but differ in that the patient may not feel sadness—rather, emotional capacity itself is diminished (Nevid et al., 2014).
Cognitive Symptoms
Cognitive impairments significantly impact daily functioning and are major predictors of disability. These include:
- Impaired attention and concentration
- Memory deficits
- Difficulty planning or solving problems
- Reduced ability to interpret social cues
- Slowed processing speed
- Poor insight into illness (anosognosia)
These deficits influence academic and employment failure even after positive symptoms are controlled.
Etiology of Schizophrenia
Schizophrenia has a multifactorial etiology, arising from the interaction of biological, psychological, and social forces. No single cause is sufficient.
Biological Etiology

Underlying Neurobiological Mechanisms of Psychosis
Genetic Factors
Twin, adoption, and family studies show strong heredity:
- 1% general population rate
- 10% among first-degree relatives
- 46% concordance among identical twins (Barlow & Durand, 2005)
However, genetics increase vulnerability rather than determine fate, supporting a diathesis-stress model.
Neurochemical Factors
The dopamine hypothesis proposes overactivity in dopamine pathways:
- Excess dopamine in mesolimbic pathway → positive symptoms
- Dopamine underactivity in mesocortical pathway → negative and cognitive symptoms (Butcher et al., 2014)
Recent research implicates:
- Glutamate dysregulation, especially NMDA receptor malfunction
- Serotonin imbalance, explaining atypical antipsychotic effectiveness
Brain Structure Abnormalities
Neuroimaging studies reveal:
- Enlarged lateral ventricles
- Reduced prefrontal cortex and temporal lobe volume
- Hippocampal abnormalities
- Reduced neural connectivity (Carson et al., 2007)
These findings support a neurodevelopmental model.
Prenatal and Birth Factors
Risk increases with:
- Maternal viral infections (influenza, rubella)
- Obstetric complications such as hypoxia
- Maternal malnutrition
- Low birth weight
- Advanced paternal age (Nevid et al., 2014)
Psychological Etiology
- Distorted cognition and misinterpretation of internal sensations intensify psychosis (Andrew, 2011).
- Poor coping strategies and emotional regulation difficulties increase breakdown during stress.
Environmental and Social Etiology
- High expressed emotion families (criticism, hostility, overinvolvement) dramatically increase relapse (Sarason & Sarason, 2002).
- Urban upbringing doubles risk.
- Migration, discrimination, and isolation increase vulnerability.
- Childhood trauma, abuse, and neglect correlate strongly with early psychosis (Sue, Sue & Sue, 2006).
Substance abuse, especially cannabis during adolescence, increases risk and worsens prognosis.
Treatment of Schizophrenia
Schizophrenia treatment requires a comprehensive, multimodal approach combining medication, psychosocial support, and rehabilitation rather than relying solely on pharmacology.
Biological Treatments
Antipsychotic Medications
Medication is the primary treatment because it stabilizes dopamine function.
First-Generation (Typical) Antipsychotics
Examples: Haloperidol, Fluphenazine, Chlorpromazine
Benefits:
Reduce positive symptoms
Limitations:
- Less effective for negative symptoms
- Higher risk of extrapyramidal side effects (tremors, rigidity)
- Tardive dyskinesia risk with long-term use (Butcher et al., 2014)
Second-Generation (Atypical) Antipsychotics
Examples: Clozapine, Risperidone, Olanzapine, Quetiapine
Benefits:
- Effective for positive and negative symptoms
- Fewer movement side effects
- Better cognitive outcomes
Limitations:
- Weight gain, metabolic syndrome
- Clozapine requires monitoring due to risk of agranulocytosis (APA, 2013)
Long-Acting Injectable Antipsychotics
Used for poor medication adherence and relapse prevention.
Electroconvulsive Therapy (ECT)
Used in cases involving severe catatonia or treatment resistance (Carson et al., 2007).
Psychosocial Treatments
Cognitive-Behavioral Therapy (CBT)
- Reduces distress associated with hallucinations and delusions
- Helps patients test reality and develop insight
- Improves functioning and reduces relapse (Nevid et al., 2014)
Family Therapy
- Lowers expressed emotion
- Improves communication and problem-solving
- Reduces hospitalization frequency
Social Skills Training
- Enhances interpersonal functioning and self-care skills
- Reduces social withdrawal
Cognitive Remediation Therapy
Improves memory, attention, and executive functioning
Psychoeducation
Increases insight and medication compliance
Supported Employment & Vocational Rehabilitation
Helps patients return to meaningful work roles
Assertive Community Treatment (ACT)
Intensive case management for high-risk individuals
Recovery and Prognosis
Although schizophrenia is chronic, many individuals achieve substantial recovery. Positive outcomes are associated with:
- Early intervention
- Strong family and social support
- Adherence to treatment
- Absence of severe negative symptoms
Recovery models emphasize hope, personal agency, and quality of life rather than full symptom removal.
Conclusion
Schizophrenia is a complex psychiatric disorder involving profound disturbances in thought, perception, emotion, and behavior. Its development is influenced by a combination of genetic predisposition, neurobiological abnormalities, psychological vulnerabilities, and environmental stress factors. While schizophrenia has historically carried pessimistic expectations, modern treatment combining antipsychotic medication with psychosocial interventions significantly improves functioning and long-term prognosis. Early intervention, rehabilitation, and community-focused recovery models enable many affected individuals to live meaningful and productive lives.
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Andrew, M. (2011). Clinical Psychology: Science, Practice, and Culture (2nd ed.). Sage.
Alloy, L. B., Riskind, J. H., & Manos, M. J. (2005). Abnormal Psychology. Tata McGraw-Hill.
Barlow, D. H., & Durand, V. M. (2005). Abnormal Psychology (4th ed.). Books/Cole.
Butcher, J. N., Mineka, S., & Hooley, J. M. (2014). Abnormal Psychology (15th ed.). Pearson.
Carson, R. C., Butcher, J. N., Mineka, S., & Hooley, J. M. (2007). Abnormal Psychology (13th ed.). Pearson.
Nevid, J. S., Rathus, S. A., & Greene, B. (2014). Abnormal Psychology (9th ed.). Pearson.
Sarason, I. G., & Sarason, R. B. (2002). Abnormal Psychology (10th ed.). Pearson Education.
Sue, D., Sue, D. W., & Sue, S. (2006). Abnormal Behavior (8th ed.). Houghton Mifflin.
World Health Organization. (2019). ICD-11 International Classification of Diseases.
Niwlikar, B. A. (2025, November 24). Schizophrenia: Definition, 3 Important Phases, Symptoms, Etiology, and Treatments. Careershodh. https://www.careershodh.com/schizophrenia-symptoms-etiology-and-treatments/
