Introduction
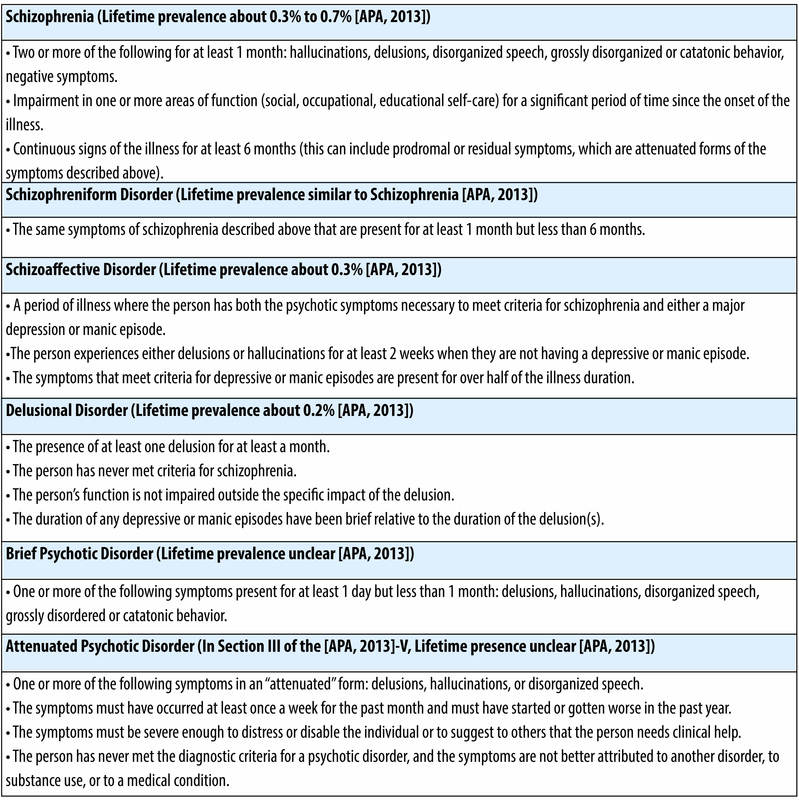
Psychotic disorders represent a class of severe mental conditions characterized primarily by a disruption in thought processes, impaired reality testing, perceptual disturbances, and disorganized behavior. Although schizophrenia is the most well-known psychotic disorder, modern diagnostic systems such as the DSM-5 (American Psychiatric Association, 2013) and ICD-11 (World Health Organization, 2019) conceptualize psychotic disorders along a spectrum. These disorders vary in terms of severity, duration, symptomatology, degree of functional impairment, and long-term prognosis, yet they share overlapping clinical and biological features.

Schizophrenia Spectrum
The major disorders grouped under the Schizophrenia Spectrum include Brief Psychotic Disorder, Schizotypal Personality Disorder, Schizophreniform Disorder, Schizoaffective Disorder, and Delusional Disorder. These conditions involve abnormalities in perception (hallucinations), belief formation (delusions), thought and language organization, emotional expression, and interpersonal functioning. The importance of distinguishing between them lies in appropriate treatment planning, prognosis estimation, and prevention of progression to more chronic forms such as schizophrenia.
Schizophrenia Spectrum Disorders
Read More: Psychodynamics
1. Brief Psychotic Disorder
Brief Psychotic Disorder is defined in DSM-5 as a disorder involving a sudden onset of at least one of the following symptoms: delusions, hallucinations, disorganized speech, or grossly disorganized or catatonic behavior, lasting for at least one day but less than one month, followed by full recovery to the individual’s premorbid functioning (APA, 2013). This short-term psychotic reaction commonly follows an intense stressor, which is why it is sometimes referred to as brief reactive psychosis.
Symptoms
Brief Psychotic Disorder symptoms emerge abruptly and intensely without early warning signs.
Positive Symptoms
These involve additions to normal functioning:
- Delusions – often persecutory or paranoid; believing others intend harm
- Hallucinations – most commonly auditory voices (Butcher, Mineka & Hooley, 2014)
- Disorganized Speech – incoherence, loose associations, derailment
- Disorganized or Catatonic Behavior – agitation, irrelevant movement, rigidity, or immobility
Emotional Disturbance
- Extreme fear or anxiety
- Sudden crying or laughter inappropriate to context
- Confusion or depersonalization
Functional Impairment
Occupational and social functioning may collapse temporarily despite eventual recovery.
Etiology
The causes of Brief Psychotic Disorder are multifactorial:
- Stress Vulnerability Model: Severe stress such as bereavement, accidents, violence, or natural disaster may precipitate an episode (Sarason & Sarason, 2002).
- Genetic Susceptibility: Higher occurrence among individuals with a family history of schizophrenia or mood disorders (Barlow & Durand, 2005).
- Cultural and Social Factors: More frequently observed among migrants, refugees, and populations under extreme sociocultural strain (Sue, Sue & Sue, 2006).
- Substance Use: Cannabis, stimulants, amphetamines, and hallucinogens can trigger psychosis.
Treatment
- Pharmacotherapy: Antipsychotics such as haloperidol or risperidone during acute phase (APA, 2013)
- Psychotherapy: Crisis intervention like cognitive-behavioral strategies for coping with stress and family education to reduce relapse risk (Nevid, Rathus & Greene, 2014)
- Prognosis: Generally excellent with full remission expected within weeks when treated properly.
2. Schizotypal Personality Disorder
Schizotypal Personality Disorder (STPD) is defined by pervasive social and interpersonal deficits, marked discomfort with close relationships, and the presence of cognitive or perceptual distortions as well as eccentric behavior. These individuals frequently appear odd or peculiar but do not typically lose contact with reality (American Psychiatric Association, 2013).
Symptoms
Symptoms develop gradually, typically during adolescence or early adulthood.
Interpersonal and Social Deficits
- Lack of close relationships
- Social withdrawal and severe anxiety in social situations
- Paranoid fears of being judged or harmed (Carson, Butcher, Mineka & Hooley, 2007)
Cognitive and Perceptual Disturbances
- Magical thinking (e.g., belief in telepathy or supernatural influence)
- Ideas of reference
- Unusual perceptual experiences such as sensing invisible presences (Butcher et al., 2014)
Behavioral and Emotional Eccentricity
- Odd mannerisms, unusual clothing styles
- Speech that is vague, metaphorical, overly elaborate
- Constricted or inappropriate emotional expression
Etiology
- Genetic Link: More common among first-degree relatives of people with schizophrenia (Barlow & Durand, 2005).
- Neurological Factors: Deficits in working memory, sustained attention, and information processing similar to schizophrenia (Nevid et al., 2014).
- Developmental Factors: Childhood neglect, emotional abuse, and social rejection commonly reported (Sarason & Sarason, 2002).
Treatment
- Psychotherapy: Supportive psychotherapy to reduce social anxiety, cognitive restructuring to challenge odd beliefs, and social skills training
- Medication: Low-dose antipsychotics may reduce cognitive distortions and improve communication (APA, 2013).
- Prognosis: Usually chronic but stable; minority may progress to schizophrenia.
3. Schizophreniform Disorder
Schizophreniform Disorder involves schizophrenia-like symptoms, lasting at least one month but less than six months. If symptoms exceed six months, the diagnosis typically changes to schizophrenia (APA, 2013).
Symptoms
Positive Symptoms
Delusions
Hallucinations
Disorganized speech
Disorganized or catatonic behavior
Negative Symptoms
Affective flattening
Alogia (reduced speech)
Avolition (lack of motivation)
Social withdrawal
Cognitive Symptoms
Impaired attention
Reduced planning and judgment ability (Nevid et al., 2014)
Etiology
- Genetic Factors: Strong familial linkage with schizophrenia and bipolar disorder (Carson et al., 2007).
- Neurobiological Factors: Brain imaging shows enlarged ventricles and reduced gray matter similar to schizophrenia (Butcher et al., 2014).
- Environmental Stressors: Trauma, urban poverty, and drug use increase risk.
Treatment
- Pharmacological: Antipsychotics (especially atypical antipsychotics)
- Psychosocial Interventions: Cognitive-behavioral therapy, family-based education supportive therapy, and skills training for work and self-care (Sarason & Sarason, 2002)
- Prognosis: One-third fully recover, while two-thirds progress to schizophrenia or schizoaffective disorder.
4. Schizoaffective Disorder
Schizoaffective Disorder combines features of schizophrenia with prominent mood disorder symptoms. Psychotic symptoms must occur for at least two weeks without mood disturbance, distinguishing it from mood-congruent psychosis (APA, 2013).
Symptoms
Psychotic Symptoms
Hallucinations
Delusions
Disorganized thinking
Catatonia
Mood Episodes
Depressive type: hopelessness, suicidal ideation
Bipolar type: manic excitement, grandiosity, decreased need for sleep (Butcher et al., 2014)
Negative Symptoms
Flat affect
Poor social functioning
Lack of pleasure or drive
Etiology
- Genetic Predisposition: Family history often includes both schizophrenia and bipolar disorder.
- Neurochemical Imbalance: Dopamine, serotonin, and norepinephrine abnormalities (Nevid et al., 2014).
- Stress and Substance Abuse: Cannabis and trauma significantly increase risk.
Treatment
- Medication: Antipsychotics (e.g., paliperidone), mood stabilizers such as lithium or valproate, and antidepressants used cautiously (APA, 2013)
- Psychotherapy: CBT, social skills and vocational training, and family therapy (Carson et al., 2007)
- Prognosis: Better than schizophrenia but worse than mood disorders; relapse is common without adherence.
5. Delusional Disorder
Delusional Disorder involves persistent non-bizarre delusions lasting at least one month without other major psychotic symptoms or significant impairment in overall functioning (APA, 2013).
Symptoms
Delusion Types
Persecutory: belief of being mistreated or conspired against
Grandiose: belief of special status, abilities, or divine mission
Erotomanic: belief that someone, usually powerful or famous, is in love with them
Jealous: belief in partner’s unfaithfulness without cause
Somatic: belief of physical illness or infestation
Behavioral Patterns
Individuals appear normal unless discussing delusional topic.
Etiology
- Personality traits such as suspiciousness and hypersensitivity (Sarason & Sarason, 2002)
- Social isolation and rigid belief systems
- Sensory impairments, particularly in older adults
Treatment
- Psychotherapy: Cognitive restructuring to challenge false beliefs, supportive therapy instead of confrontation, and family education (Barlow & Durand, 2005)
- Pharmacotherapy: Antipsychotic medications may reduce delusional intensity.
- Prognosis: Generally good; individuals remain functional with minimal impairment.
Conclusion
The Schizophrenia Spectrum encompasses a range of disorders that share fundamental disturbances in thinking, perception, emotional processing, and behavioral regulation. Although they differ in severity and clinical course, understanding their distinctions is essential for effective diagnosis and treatment. Early intervention, integrated therapy, medication adherence, and psychosocial support greatly improve outcomes across all disorders in the spectrum.
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Andrew, M. (2011). Clinical Psychology: Science, Practice, and Culture (2nd ed.). Sage Publications.
Alloy, L. B., Riskind, J. H., & Manos, M. J. (2005). Abnormal Psychology. Tata McGraw-Hill.
Barlow, D. H., & Durand, V. M. (2005). Abnormal Psychology (4th ed.). Books/Cole.
Butcher, J. N., Mineka, S., & Hooley, J. M. (2014). Abnormal Psychology (15th ed.). Pearson.
Carson, R. C., Butcher, J. N., Mineka, S., & Hooley, J. M. (2007). Abnormal Psychology (13th ed.). Pearson.
Nevid, J. S., Rathus, S. A., & Greene, B. (2014). Abnormal Psychology (9th ed.). Pearson.
Sarason, I. G., & Sarason, R. B. (2002). Abnormal Psychology (10th ed.). Pearson.
Sue, D., Sue, D. W., & Sue, S. (2006). Abnormal Behavior (8th ed.). Houghton Mifflin.
World Health Organization. (2019). ICD-11 International Classification of Diseases.
Niwlikar, B. A. (2025, November 25). 5 Important Schizophrenia Spectrum Disorders. Careershodh. https://www.careershodh.com/5-important-schizophrenia-spectrum-disorders/
