Introduction
Traumatic stress disorders arise following exposure to stressful or traumatic events that overwhelm an individual’s ability to cope (APA, 2013). These disorders significantly impair emotional, cognitive, and social functioning. Among the most recognized are Post-Traumatic Stress Disorder (PTSD), Acute Stress Disorder (ASD), and Adjustment Disorders (AD). While all involve maladaptive responses to stress, they differ in onset, duration, symptomatology, and diagnostic criteria. Understanding their clinical features, etiology, and treatment approaches is essential for effective psychological and psychiatric care.
Read More: ICD vs DSM
Post-Traumatic Stress Disorder (PTSD)
Post-Traumatic Stress Disorder is a severe anxiety disorder that develops after exposure to traumatic events such as violence, natural disasters, accidents, or war. PTSD is characterized by intrusive thoughts, avoidance behaviors, negative alterations in cognition and mood, and hyperarousal (APA, 2013; Barlow & Durand, 2005). Unlike typical stress responses, PTSD symptoms persist for more than a month and significantly impair functioning.
Diagnostic Criteria
According to the DSM-5, PTSD is diagnosed when the following criteria are met:
- Exposure to a traumatic event: Direct experience, witnessing, learning about trauma to a close family member/friend, or repeated exposure to aversive details of trauma.
- Presence of intrusion symptoms:
- Recurrent, involuntary, and intrusive distressing memories.
- Traumatic nightmares.
- Flashbacks or dissociative reactions.
- Persistent avoidance: Efforts to avoid distressing memories, thoughts, feelings, or external reminders.
- Negative alterations in cognition and mood:
- Inability to remember trauma details.
- Persistent negative beliefs about oneself or the world.
- Distorted blame, persistent negative emotional state.
- Marked alterations in arousal and reactivity: Irritability, reckless behavior, hypervigilance, exaggerated startle response.
- Duration of symptoms: More than one month.
- Functional impairment: Clinically significant distress or social/occupational impairment.
- Not attributable to substance use or medical conditions (APA, 2013; Comer, 2007).
Etiology
PTSD arises from a complex interaction of biological, psychological, and social factors:
- Traumatic exposure: Severity, duration, and proximity of trauma are strong predictors.
- Genetic vulnerability: Family history of anxiety or mood disorders increases risk.
- Neurobiological factors: Dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis and amygdala hyperactivity contribute to hyperarousal and intrusive memories.
- Cognitive and personality factors: Negative appraisal of trauma, low resilience, and maladaptive coping strategies increase susceptibility.
- Environmental factors: Lack of social support, ongoing stressors, or previous trauma exacerbate symptom development (Andrew, 2011; Alloy, Riskind, & Manos, 2005; Nevid, Rathus, & Greene, 2014).

HPA Axis in PTSD
Clinical Features
PTSD manifests through clusters of symptoms:
- Intrusive re-experiencing: Flashbacks, nightmares, distressing memories.
- Avoidance behaviors: Avoiding reminders of trauma, emotional numbing.
- Negative mood and cognition: Feelings of guilt, shame, or detachment.
- Arousal and reactivity: Sleep disturbances, hypervigilance, irritability (Barlow & Durand, 2005; Carson et al., 2007).
Chronic PTSD can lead to comorbid depression, substance use, or suicidal ideation.
Treatment and Interventions
Evidence-based treatment for PTSD includes:
- Cognitive Behavioral Therapy (CBT): Trauma-focused CBT emphasizes exposure to traumatic memories and cognitive restructuring.
- Eye Movement Desensitization and Reprocessing (EMDR): Combines eye movement with exposure therapy to reduce distress.
- Pharmacotherapy: Selective Serotonin Reuptake Inhibitors (SSRIs) are first-line medications.
- Stress inoculation training: Teaches coping strategies for managing anxiety and hyperarousal.
- Supportive psychotherapy: Enhances social support and addresses secondary stressors (Butcher, Mineka, & Hooley, 2014; Sue, Sue, & Sue, 2006).
Early intervention post-trauma reduces chronicity and improves functional outcomes.
Acute Stress Disorder (ASD)
Acute Stress Disorder is a transient anxiety disorder occurring immediately after a traumatic event, lasting 3 days to 4 weeks. ASD symptoms resemble PTSD but are shorter in duration and may resolve without treatment. Early identification is essential, as ASD can be a precursor to PTSD if symptoms persist (APA, 2013; Barlow & Durand, 2005).
Treatment for Acute Stress Disorder
Diagnostic Criteria
DSM-5 criteria for ASD include:
- Exposure to trauma: Similar to PTSD criteria.
- Presence of nine or more symptoms from five categories:
- Intrusion: Flashbacks, distressing memories.
- Negative mood: Persistent fear or helplessness.
- Dissociation: Altered sense of reality, depersonalization.
- Avoidance: Efforts to avoid trauma reminders.
- Arousal: Sleep disturbances, hypervigilance, irritability.
- Duration: 3 days to 4 weeks post-trauma.
- Functional impairment: Clinically significant distress or impairment.
- Exclusion of other disorders (APA, 2013; Andrew, 2011).
Etiology
ASD shares risk factors with PTSD but emphasizes immediate psychological response:
- Severity and proximity of trauma exposure.
- Pre-existing anxiety or depression.
- Lack of social support.
- Cognitive appraisal: Individuals perceiving trauma as catastrophic are at higher risk.
- Biological predisposition: Genetic and neurochemical factors may influence acute stress responses (Alloy, Riskind, & Manos, 2005; Nevid et al., 2014).
Clinical Features
Key ASD symptoms include:
- Intrusive thoughts, flashbacks, and nightmares.
- Dissociation: Feeling detached or unreal.
- Anxiety and hyperarousal.
- Avoidance of trauma-related stimuli.
- Emotional numbing or irritability (Barlow & Durand, 2005; Carson et al., 2007).
If symptoms persist beyond four weeks, the diagnosis may transition to PTSD.
Treatment and Interventions
Effective interventions for ASD aim to prevent progression to PTSD:
- Psychological First Aid (PFA): Immediate support post-trauma to stabilize the individual.
- CBT: Early trauma-focused CBT reduces symptom severity.
- Relaxation techniques: Mindfulness, deep breathing, and stress reduction strategies.
- Pharmacotherapy: Short-term use of anxiolytics may be considered for severe symptoms (Sue, Sue, & Sue, 2006; Butcher, Mineka, & Hooley, 2014).
Prompt intervention is associated with better prognosis and reduced risk of chronic PTSD.
Adjustment Disorders (AD)
Adjustment Disorders are maladaptive emotional or behavioral responses to identifiable stressors, occurring within 3 months of the stressor onset (APA, 2013). Unlike PTSD or ASD, the stressor may be non-traumatic, such as job loss, illness, or interpersonal conflict. AD is distinguished by excessive distress or functional impairment relative to the stressor’s severity.
Adjustment Disorder
Diagnostic Criteria
DSM-5 criteria include:
- Development of emotional or behavioral symptoms in response to an identifiable stressor.
- Symptoms within 3 months of stressor onset.
- Clinically significant distress or impairment in social, occupational, or academic functioning.
- Not an exacerbation of another mental disorder.
- Symptoms do not persist beyond 6 months after stressor termination (APA, 2013; Alloy, Riskind, & Manos, 2005).
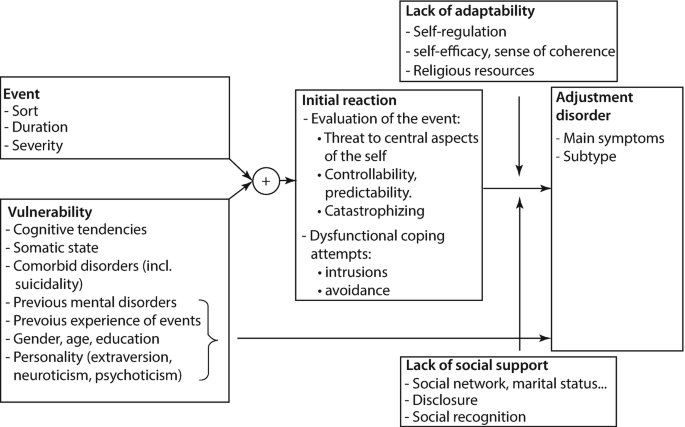
Etiology
Adjustment Disorders arise from stressors that exceed an individual’s coping capacity:
- Environmental stressors: Life transitions, losses, financial problems.
- Personality and coping style: Low resilience, poor coping strategies.
- Social support: Lack of emotional or practical support increases vulnerability (Andrew, 2011; Barlow & Durand, 2005).
Clinical Features
Symptoms vary but typically include:
- Depressed mood, anxiety, or irritability.
- Social withdrawal or difficulty functioning at work/school.
- Somatic complaints: Headaches, gastrointestinal distress.
- Behavioral disturbances: Aggression, risk-taking, or impulsivity (Carson et al., 2007; Nevid et al., 2014).
Symptoms are proportional to stressor severity but cause notable impairment.
Treatment and Interventions
Adjustment Disorders respond well to short-term psychotherapy:
- Cognitive Behavioral Therapy (CBT): Enhances coping skills and reframes maladaptive thoughts.
- Supportive therapy: Emotional support and problem-solving guidance.
- Stress management: Relaxation training, time management, and lifestyle modifications.
- Pharmacotherapy: Reserved for severe anxiety or depressive symptoms (Butcher, Mineka, & Hooley, 2014; Sue, Sue, & Sue, 2006).
With timely intervention, prognosis is generally good, and symptoms often resolve once stressors are managed or removed.
Conclusion
Traumatic stress disorders encompass a spectrum of maladaptive responses to stressors and trauma. PTSD represents chronic, severe trauma response, ASD denotes immediate, short-term reactions, and Adjustment Disorders involve maladaptive coping to identifiable stressors. Early recognition, accurate diagnosis, and evidence-based interventions are essential to prevent long-term impairment. Treatments such as CBT, EMDR, supportive therapy, and pharmacological management provide effective strategies to reduce symptoms and enhance functioning. A comprehensive understanding of these disorders equips clinicians to support individuals in navigating traumatic and stressful experiences effectively.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
Alloy, L. B., Riskind, J. H., & Manos, M. J. (2005). Abnormal psychology: Current perspectives (9th ed.). New Delhi, India: Tata McGraw-Hill.
Andrew, M. (2011). Clinical psychology: Science, practice, and culture (2nd ed.). Sage Publications.
Barlow, D. H., & Durand, V. M. (2005). Abnormal psychology (4th ed.). Pacific Grove, CA: Books/Cole.
Butcher, J. N., Mineka, S., & Hooley, J. M. (2014). Abnormal psychology (15th ed.). Delhi: Dorling Kindersley (India) Pvt. Ltd.
Carson, R. C., Butcher, J. N., Mineka, S., & Hooley, J. M. (2007). Abnormal psychology (13th ed.). India: Pearson Education.
Comer, R. J. (2007). Abnormal psychology (6th ed.). New York: Worth Publishers.
Nevid, J. S., Rathus, S. A., & Greene, B. (2014). Abnormal psychology (9th ed.). Pearson Education.
Sue, D., Sue, D. W., & Sue, S. (2006). Abnormal behavior (8th ed.). Houghton Mifflin Company.
Niwlikar, B. A. (2025, October 1). 3 Important Traumatic Stress Disorders: Post-Traumatic Stress Disorder (PTSD), Acute Stress Disorder, and Adjustment Disorders. Careershodh. https://www.careershodh.com/traumatic-stress-disorders/
