Introduction
The field of mental health has undergone significant evolution over the last century, influenced by scientific advances, sociocultural changes, and shifting legal frameworks. Mental health professionals play a crucial role in identifying, treating, rehabilitating, and preventing psychological disorders, while also promoting psychological well-being at both individual and community levels. Their responsibilities are not limited to clinical practice but extend into advocacy, research, education, and policymaking.
The DSM-5 (American Psychiatric Association, 2013) and ICD-10 (World Health Organization, 1992) provide the diagnostic frameworks that guide practice globally. In India, the Mental Health Care Act, 2017 highlights the importance of patient rights, community-based rehabilitation, and de-stigmatization, reshaping the expectations and responsibilities of professionals in the field.

DSM vs ICD
1. Psychiatrists
Psychiatrists are medical doctors who specialize in the prevention, diagnosis, and treatment of mental disorders. Their core responsibilities include:
- Diagnosis: Psychiatrists rely on structured interviews and diagnostic frameworks like the DSM-5 to classify mental illnesses. For instance, schizophrenia, characterized by delusions and hallucinations, is diagnosed through careful symptom mapping.
- Pharmacotherapy: Psychiatrists prescribe and monitor medications such as antipsychotics, antidepressants, anxiolytics, and mood stabilizers. According to Barlow & Durand (2005), effective management often requires adjusting dosages, addressing side effects, and ensuring adherence.
- Hospitalization: They oversee inpatient care for severe cases (e.g., acute psychosis, suicidal crises).
- Liaison Role: Psychiatrists collaborate with other medical professionals, recognizing the interplay of physical and mental health (e.g., depression in chronic illness).
Their dual training in medicine and psychiatry positions them uniquely to integrate biological, psychological, and social perspectives in treatment.
2. Clinical Psychologists
Clinical psychology, as defined by Andrew (2011), integrates science and practice to understand, prevent, and alleviate maladjustment. Clinical psychologists’ responsibilities are diverse:
- Assessment and Testing: They use standardized psychometric instruments (e.g., MMPI, Rorschach, intelligence tests) to assess personality, cognition, and functioning (Butcher, Mineka, & Hooley, 2014).
- Therapeutic Interventions: They provide psychotherapy using evidence-based modalities such as cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), psychodynamic therapy, and humanistic-existential approaches.
- Research Contributions: Clinical psychologists actively engage in developing and evaluating therapeutic interventions, contributing to evidence-based practice.
- Consultation: They provide expertise in schools, courts, rehabilitation centers, and industries, broadening the scope of mental health services.
Unlike psychiatrists, they do not typically prescribe medication, but their psychological interventions often complement pharmacological treatments.
3. Counselors and Psychotherapists
Counselors focus on mild-to-moderate concerns such as stress, relationship issues, grief, or adjustment problems. Their role, as Comer (2007) notes, is rooted in the humanistic paradigm that emphasizes self-exploration and personal growth.
- Supportive Counseling: Through active listening and empathy, counselors create safe environments for clients to articulate their problems.
- Goal Setting: They assist clients in setting realistic, achievable goals for coping and adjustment.
- Short-Term Interventions: Unlike long-term psychoanalysis, counseling is often solution-focused and time-limited.
Counselors are vital for early intervention, preventing escalation into severe psychopathology.
4. Psychiatric Social Workers
Psychiatric social workers (PSWs) play an indispensable role in addressing the social determinants of mental health. According to Sarason & Sarason (2002), their work ensures that patients’ recovery is not hindered by environmental stressors.
- Resource Mobilization: PSWs help patients and families access welfare schemes, financial assistance, and rehabilitation opportunities.
- Family Counseling: They mediate family dynamics, particularly in disorders where caregiving is critical (e.g., dementia, autism).
- Reintegration: By liaising with community organizations, PSWs support reintegration of patients into employment, education, and social life.
Their holistic approach recognizes that clinical recovery must be complemented by functional and social recovery.
5. Psychiatric Nurses
Psychiatric nurses deliver hands-on care and form the backbone of mental health institutions. Their responsibilities include:
- Medication Administration: Ensuring correct dosages, monitoring side effects, and educating patients about medication adherence.
- Crisis Management: De-escalating aggressive behavior or suicide attempts, often being the first responders.
- Therapeutic Communication: Building rapport with patients, offering emotional support, and helping them adapt to routines.
- Community Outreach: Conducting mental health awareness and follow-ups in rural or underserved areas (Puri, Laking, & Treasaden, 1996).
Their continuous patient contact allows them to notice subtle behavioral changes that inform treatment adjustments.
6. Allied Professionals
Other professionals such as occupational therapists, speech therapists, and art or music therapists contribute significantly to rehabilitation. For example, occupational therapists help patients with schizophrenia regain daily living skills, while expressive therapies foster emotional release and creativity.
7. Working in Multidisciplinary Teams
Modern mental health care relies on teamwork. According to Sue, Sue, & Sue (2006), multidisciplinary collaboration ensures holistic treatment by integrating medical, psychological, and social perspectives.
- Case Conferences: Regular meetings allow professionals to share progress reports, challenges, and treatment modifications.
- Shared Responsibility: Each professional contributes distinct expertise; for example, a psychiatrist manages medication while a psychologist provides psychotherapy.
- Continuity of Care: Teams ensure smoother transitions between inpatient, outpatient, and community-based services.
Such collaborative frameworks reduce relapse rates and improve quality of life for patients.
8. Ethical Responsibilities
Ethics are foundational in mental health practice. Professionals must adhere to codes of conduct outlined by national and international bodies.
- Confidentiality: Protecting sensitive client information is paramount, though exceptions exist in cases of imminent harm.
- Informed Consent: Clients must be fully informed about treatment options and potential risks.
- Non-Discrimination: Professionals must provide culturally sensitive care, acknowledging differences in ethnicity, gender, and socioeconomic status.
- Professional Boundaries: Dual relationships (e.g., therapist-client friendships) must be avoided to prevent exploitation.
The Mental Health Care Act, 2017 (India) further emphasizes patient rights, mandating informed decision-making and dignified treatment.

Ethics Models of Mental Health Care
Read More: Mental Health and What Does It Mean?
9. Legal Responsibilities
Legal frameworks guide professional conduct and patient protection.
- Documentation: Accurate record-keeping is vital for accountability and continuity of care.
- Mandatory Reporting: Professionals must report risks of harm to self or others, and suspected abuse.
- Competency Assessments: Psychologists and psychiatrists are often called upon to evaluate mental competency in legal settings.
- Guardianship and Rights: The Mental Health Care Act establishes legal guardianship protocols, requiring professionals to balance patient autonomy with safety.
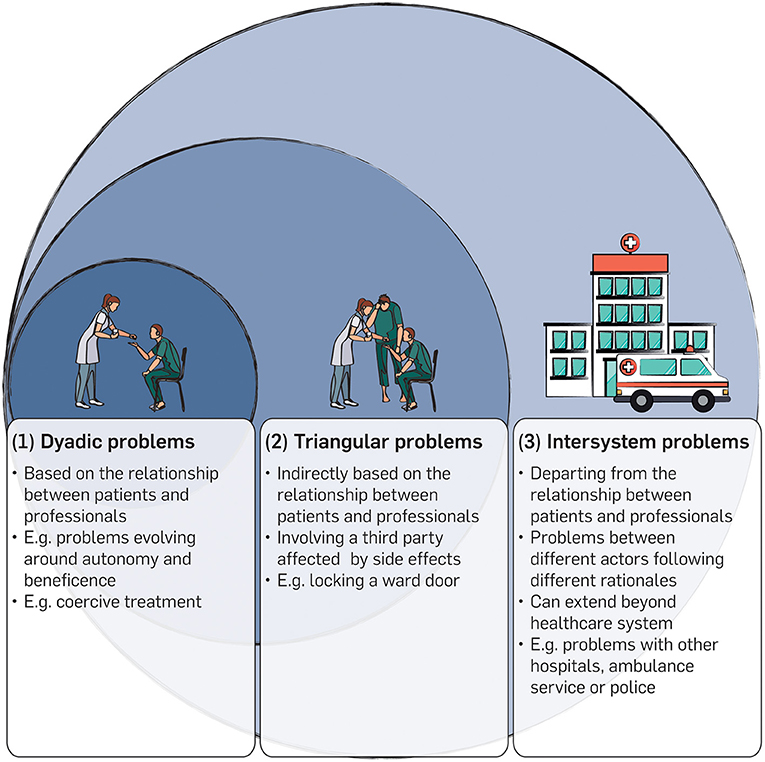
Types of Ethical Problems and Expertise in Clinical Ethics Consultation in Psychiatry
10. Research and Academic Roles
Mental health professionals advance the field by conducting research in diagnosis, treatment efficacy, epidemiology, and prevention. Nolen-Hoeksema (2004) underscores their role in developing culturally adapted interventions, particularly in non-Western contexts. Many professionals also engage in teaching, shaping future generations of practitioners.
11. Advocacy and Public Awareness
Stigma remains one of the greatest barriers to mental health care. Professionals are increasingly expected to engage in advocacy:
- Policy Advocacy: Influencing policies that expand access to mental health services.
- Public Education: Campaigns to dispel myths, encourage help-seeking, and normalize mental health discussions.
- Community Empowerment: Supporting grassroots initiatives that integrate mental health into schools, workplaces, and community centers.
By raising awareness, professionals contribute to prevention and early intervention, reducing the burden of untreated disorders.
Challenges and Future Directions
Despite their critical roles, mental health professionals face challenges such as understaffing, burnout, stigma, and limited resources—particularly in low- and middle-income countries. The future demands:
- Task-Shifting: Training community health workers to deliver basic interventions.
- Tele-Mental Health: Expanding access through digital platforms, especially post-COVID-19.
- Cultural Adaptation: Ensuring interventions respect cultural values and norms.
- Global Collaboration: Integrating WHO guidelines with local practices for comprehensive care.
Conclusion
The roles and responsibilities of mental health professionals are multidimensional, requiring a delicate balance between clinical expertise, ethical integrity, legal accountability, research, and advocacy. Whether prescribing medication, conducting therapy, providing family support, or advocating for systemic reforms, these professionals form the backbone of mental health systems worldwide. Grounded in diagnostic frameworks like the DSM-5 and supported by legislation such as the Mental Health Care Act, 2017, they remain indispensable agents in the pursuit of psychological well-being and human dignity.
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: APA.
Andrew, M. (2011). Clinical psychology: Science, practice, and culture (2nd ed.). Sage.
Barlow, D.H., & Durand, V.M. (2005). Abnormal psychology (4th ed.). Brooks/Cole.
Butcher, J.N., Mineka, S., & Hooley, J.M. (2014). Abnormal Psychology (15th ed.). Pearson.
Comer, R.J. (2007). Abnormal psychology (6th ed.). Worth Publishers.
Puri, B.K., Laking, P.J., & Treasaden, I.H. (1996). Textbook of psychiatry. Churchill Livingston.
Sarason, I.G., & Sarason, R.B. (2002). Abnormal psychology: The problem of maladaptive behavior (10th ed.). Pearson.
Sue, D., Sue, D.W., & Sue, S. (2006). Abnormal behavior (8th ed.). Houghton Mifflin.
World Health Organization. (1992). The ICD-10 Classification of Mental and Behavioral Disorders. Oxford University Press.
The Mental Health Care Act. (2017). Government of India.
Nolen-Hoeksema, S. (2004). Abnormal Psychology (3rd ed.). McGraw-Hill.
Niwlikar, B. A. (2025, September 17). Mental Health Professionals and Their 6 Important Role and Responsibilities. Careershodh. https://www.careershodh.com/responsibilities-mental-health-professionals/
