Introduction
Aging is not solely a biological process but also a psychosocial journey that often entails vulnerabilities to mental health problems. While many older adults age successfully and remain psychologically resilient, a substantial proportion experience mental health disorders. Anxiety, depression, substance abuse, and psychotic disorders present unique challenges in old age due to the interplay of biological decline, psychosocial stressors, and cultural perceptions of aging.
These conditions often coexist with physical illnesses, leading to underdiagnosis and undertreatment. Understanding disorders of aging is crucial for designing interventions that promote mental health, enhance quality of life, and reduce the stigma surrounding mental illness in elderly populations.
Read More: Geropsychology
1. Anxiety Disorders in Aging
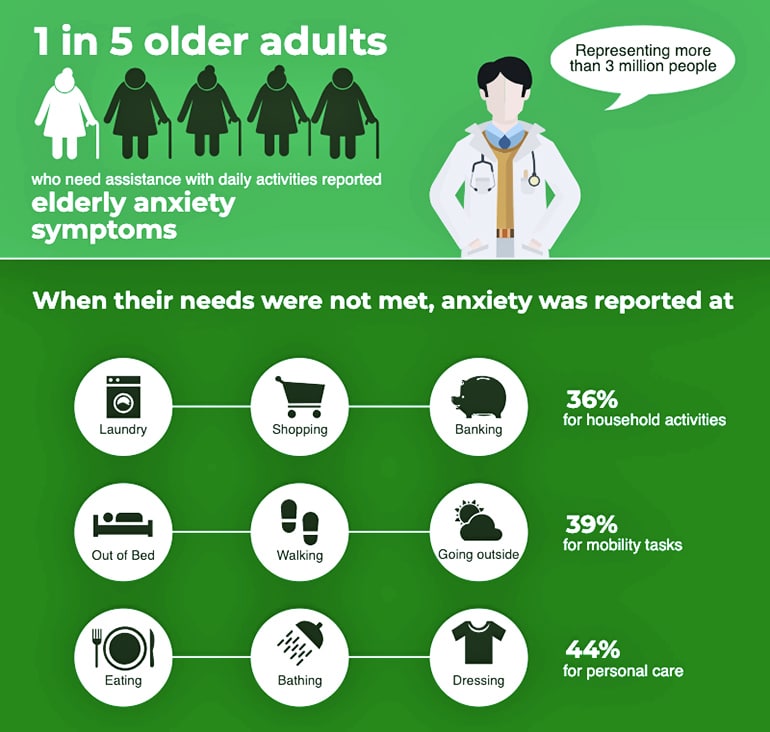
Anxiety is one of the most common psychological disorders in older adults, though it often goes unrecognized. Older adults may not present with the classic symptoms of worry or panic; instead, anxiety often manifests as somatic complaints such as muscle tension, gastrointestinal issues, or sleep disturbances (Comer, 2007).
Anxiety in Aging
Contributing Factors
- Physical Health Decline: Chronic illnesses such as heart disease, diabetes, and arthritis can exacerbate anxiety (Birren & Schaie, 2001).
- Life Transitions: Retirement, bereavement, reduced independence, and relocation to assisted living facilities are significant stressors (Elizabeth, 1981).
- Cognitive Decline: Mild cognitive impairment or early dementia may contribute to heightened fears and uncertainty.
Impact
Anxiety in the elderly often reduces quality of life, exacerbates physical symptoms, and complicates the management of chronic illnesses. Feldman and Babu (2011) argue that untreated anxiety increases the risk of depression and accelerates functional decline.
Treatment
Psychotherapeutic approaches such as cognitive-behavioral therapy (CBT), relaxation training, and exposure therapies are effective even in late life. Pharmacological treatments, including selective serotonin reuptake inhibitors (SSRIs), may be used cautiously due to sensitivity to side effects (Schulz, 2006).
2. Depression in Aging
Depression is one of the most prevalent mental health disorders in late life. Unlike depression in younger adults, late-life depression is often masked by physical complaints such as fatigue, loss of appetite, or sleep problems. This makes it difficult to diagnose, especially when symptoms overlap with chronic illness (Taylor, 1999).

Depression in Aging
Risk Factors
- Biological: Neurochemical changes, particularly reduced serotonin and dopamine functioning, play a role.
- Psychosocial: Loneliness, social isolation, bereavement, and financial insecurity contribute significantly (Johnson & Walker, 2016).
- Medical: Chronic illnesses, especially those that reduce mobility, are linked with higher rates of depression.
Consequences
Depression increases the risk of suicide among older adults, particularly men over 65 (Comer, 2007). It also worsens outcomes for physical illnesses and reduces adherence to medical treatments.
Management
Effective treatments include antidepressant medications, psychotherapy, and social interventions. Spiritual practices and community engagement also serve as protective factors, with Johnson and Walker (2016) emphasizing the importance of spiritual resilience in late-life coping.
3. Substance Abuse in Aging
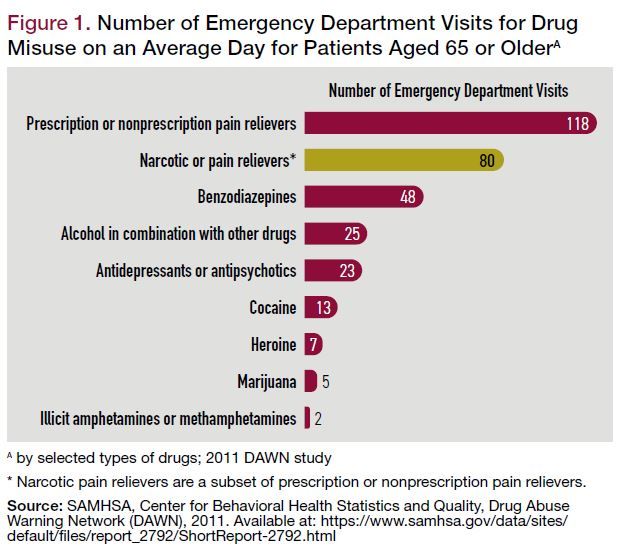
Substance abuse in the elderly is often overlooked due to stereotypes that it is primarily a younger person’s problem. However, late-onset substance abuse is increasingly recognized as a significant issue. Alcohol is the most common substance misused, followed by prescription medications such as benzodiazepines and opioids (Schulz, 2006).
Substance Abuse in Aging
Causes and Risk Factors
- Self-Medication: Older adults may use substances to cope with loneliness, pain, or sleep disturbances (Eyetsemitan & Gire, 2003).
- Access to Prescriptions: Polypharmacy increases the risk of misuse and dependence.
- Cultural Attitudes: In some societies, alcohol consumption is normalized, making recognition of abuse more difficult.
Consequences
Substance abuse accelerates physical decline, exacerbates chronic illnesses, and increases the risk of falls and injuries. It also impairs cognition, worsening confusion and memory loss (Birren & Schaie, 2001).
Treatment
Treatment approaches must be age-sensitive, considering medical comorbidities and cognitive status. Group therapy, medical detoxification, and careful monitoring of prescription drugs are effective strategies. Feldman and Babu (2011) emphasize that integrating family support enhances recovery outcomes.
4. Psychotic Disorders in Aging
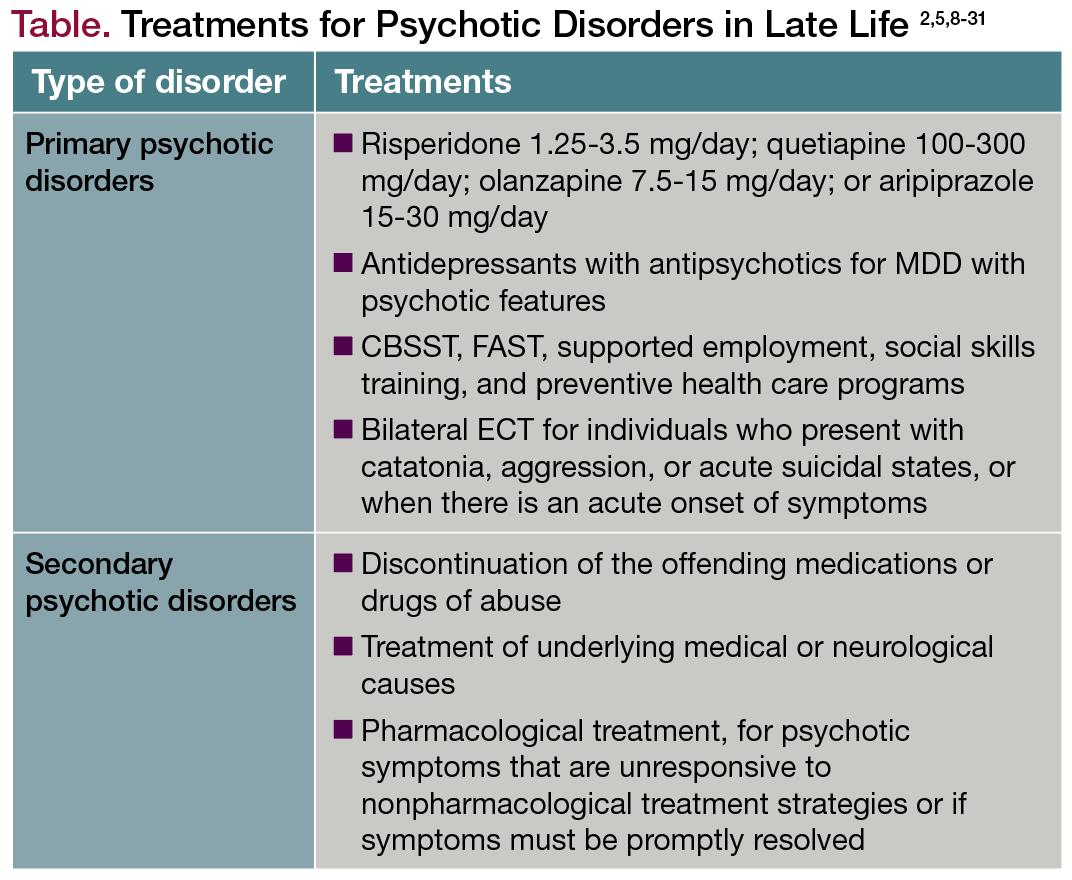
Psychotic disorders in older adults may be late-onset (developing after age 60) or the continuation of earlier-life conditions such as schizophrenia. Psychosis is characterized by hallucinations, delusions, and disorganized thinking, which significantly impair functioning (Comer, 2007).
Treatment of Psychotic Disorders in Late Life
Causes
- Neurodegenerative Diseases: Conditions such as Alzheimer’s disease and Parkinson’s disease often involve psychotic symptoms.
- Medical Conditions: Delirium, infections, and metabolic disturbances can trigger psychosis.
- Medications: Certain drugs, particularly those affecting the central nervous system, may induce psychotic symptoms in elderly patients.
Impact
Psychotic disorders in older adults increase caregiver burden and often necessitate institutional care. Social stigma further isolates those affected, exacerbating symptoms (Eyetsemitan & Gire, 2003).
Treatment
Antipsychotic medications are used but with caution, as older adults are more susceptible to side effects such as sedation and cardiovascular problems. Psychosocial interventions, including supportive therapy and structured environments, are critical for long-term management (Schulz, 2006).
Interplay Between Disorders of Aging and Physical Health
Mental health disorders in old age rarely occur in isolation. Anxiety, depression, substance abuse, and psychotic disorders often interact with physical illnesses, creating a cycle of decline. For example:
- Depression worsens the prognosis of heart disease.
- Anxiety can interfere with diabetes management.
- Substance abuse accelerates liver and kidney damage.
- Psychosis complicates treatment adherence and increases the risk of injury.
This bidirectional relationship underscores the need for integrated care models that address both mental and physical health simultaneously (Taylor, 1999).
Cultural and Social Dimensions
Aging and mental health disorders are perceived differently across cultures. In Western societies, independence and autonomy are emphasized, leading to distress when older adults lose self-sufficiency. In contrast, collectivist cultures often provide stronger family support systems, buffering against mental health challenges (Eyetsemitan & Gire, 2003).
Spirituality and meaning-making play a crucial role in coping with disorders of aging. Johnson and Walker (2016) note that spiritual engagement helps older adults reinterpret suffering, find hope, and sustain psychological resilience.
Promoting Mental Health in Aging
Some ways to promote mental health in aging include:
1. Early Detection and Diagnosis
Improving screening for anxiety, depression, substance abuse, and psychosis in primary care settings is vital, as these disorders often present with physical complaints.
2. Psychosocial Interventions
Community programs, peer support groups, and intergenerational initiatives foster social connections and reduce isolation.
3. Policy and Healthcare Systems
Policies should prioritize geriatric mental health, integrating it into broader healthcare frameworks. Training healthcare providers in age-sensitive mental health care is essential (Schulz, 2006).
4. Holistic Approaches
A holistic framework that combines medical, psychological, social, and spiritual interventions can significantly improve outcomes for older adults (Birren & Schaie, 2001).
Conclusion
Anxiety, depression, substance abuse, and psychotic disorders are critical challenges in aging populations. These disorders often remain underdiagnosed due to overlapping symptoms with physical illnesses and societal stereotypes. They are, however, highly consequential—reducing quality of life, worsening physical health, and increasing mortality risk.
By integrating medical treatment, psychosocial support, and spiritual engagement, societies can address the complex mental health needs of older adults. Promoting awareness, reducing stigma, and implementing comprehensive healthcare models are essential for ensuring that the later years of life are not only longer but also healthier and more fulfilling.
References
Birren, J. E., & Schaie, K. W. (2001). Handbook of the Psychology of Aging (5th ed.). Academic Press: London.
Comer, R. J. (2007). Abnormal Psychology (6th ed.). Worth Publishers.
Elizabeth, B. Hurlock (1981). Developmental Psychology: A Life-Span Approach (5th ed.). Tata McGraw-Hill: Delhi.
Eyetsemitan, F. E., & Gire, J. T. (2003). Aging and Adult Development in the Developing World: Applying Western Theories and Concepts. Library of Congress.
Feldman, R. S., & Babu, N. (2011). Discovering the Life Span. Pearson.
Johnson, M., & Walker, J. (2016). Spiritual Dimensions of Aging. Cambridge University Press: UK.
Schulz, R. (2006). The Encyclopaedia of Aging: A Comprehensive Resource in Gerontology and Geriatrics (4th ed.). Springer Publishing Company, Inc.
Taylor, S. E. (1999). Health Psychology (4th ed.). McGraw-Hill International (Ed.) Psychology Series.
Niwlikar, B. A. (2025, September 5). 4 Important Disorders of Aging. Careershodh. https://www.careershodh.com/disorders-of-aging/
